
Surgical treatment, complications and preventive surgery of fractures in pycnodysostosis: a systematic review
Introduction
Pycnodysostosis (PYCD) is a rare genetic disorder causing skeletal dysplasia (1). Approximately 200 affected individuals have been reported in the medical literature (2). It is inherited in an autosomal recessive manner and often recurs in families where the parents are consanguineous (1). PYCD belongs to a larger group of diseases known as lysosomal storage disorders and it is caused by a gene mutation leading cathepsin K (CTSK) deficiency (3-5). CTSK enzyme is involved in bone remodeling and highly expressed in osteoclasts resulting in abnormal storage of toxic materials in lysosomes hindering the physiological bone resorption (6,7). The severity of the disorder can vary greatly among affected individuals (8).
This condition is characterized by short-limbed short stature (9), typical facial appearance (frontal bossing, prominent nose with convex nasal ridge, midface retrusion and prominent eyes with blueish sclera) (10,11), dental abnormalities (12,13), osteosclerosis with increased bone fragility (14), brachydactyly with nail anomalies (15) and delayed closure of the cranial sutures (16,17).
Regarding laboratory findings growth hormone deficiency and low insulin-like growth factor 1 (IGF-1) levels are characteristic (18).
The diagnosis can be established in a proband with characteristic clinical and radiographic features (acro-osteolysis, generalized and progressive osteosclerosis, clavicular dysplasia and loss of the normal angle of the jaw are almost pathognomonic) (1).
The altered bone quality typical of this disease cause the bones to be fragile and brittle with the medullary canal present while often narrowed. As a result, individuals with PYCD have an increased fracture rate with an average 0.2 fractures per year (9) and delayed healing with incomplete remodeling. Surgical fixation is therefore quite challenging and often complicated by narrow medullary canals, and sclerotic bone with an increased risk of intraoperative iatrogenic fracture (19).
To date, there are no published standard treatment guidelines for PYCD nor any indication as to the best surgical intervention for fracture treatment in this condition.
The aim of our work was to systematically review the current literature available on this matter focusing on the issues and features of the management and treatment of PYCD patients with fractures. We present the following article in accordance with the Preferred Reporting Items for Systematically Reviews and Meta-Analyses (PRISMA) reporting checklist (available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-19/rc).
Methods
A systematic review of the literature indexed in PubMed, MEDLINE, and Cochrane Library databases using as search terms “pycnodysostosis fracture” was performed in January 2022. To minimize the number of missed studies, no filters were applied to the search strategy. The bibliography of the selected studies was accurately searched by hand, to identify further studies not found during the electronic search. No restrictions were applied concerning the date of publication nor the language. The title of the journal, name of authors, or supporting institutions were not masked at any stage.
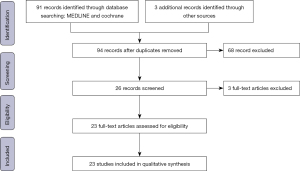
The PRISMA was followed as reported in Figure 1. In ordered to be considered for this review the articles needed to present some inclusion criteria: at least a section of the population understudy needed to be affected by PYCD, bone fracture, the treatment performed needed to be explicit. Literature focused on maxillofacial manifestations/surgery were excluded.
Abstracts and full texts were independently screened by two authors (MBB and OP), any discordance was solved by consensus with a third author (RV). The methodological quality of the studies was assessed using the modified Coleman methodology score (mCMS) (20). Each article was evaluated by two independent investigators (MBB and NB); in cases with more than a five-point difference between their rating, the discrepancy was solved by consensus with a third author (GM). The mCMS ranges from 0 to 100 points, representing a well-designed study with no bias or confounding factors. All the selected studies were retrospectively analyzed by an author (MBB) who then extracted and entered the data in an Excel worksheet. The collected data included: main author, year of publication, article type, mCMS, patient age and gender, kind of trauma, fracture number and site, fixation performed, bony union achieved and potential complications. Lastly, the data sheet was reviewed by two authors (OP and CG) who agreed on the extracted data.
Results
Demographic data
The searches resulted in 94 articles. Following the PRISMA flow chart (21), 23 articles were relevant to the general topic area and were finally included in the review (14,19,22-42) (Table 1).
Table 1
| Ref. | Year of publication | Manuscript category | mCMS | Gender | Age | |||
|---|---|---|---|---|---|---|---|---|
| M | F | ≤18 years | >18 years | |||||
| Mahmoudi et al. (22) | 2020 | Case Report | 15 | 1 | – | 1 | – | |
| Grewal et al. (19) | 2019 | Case Series | 29 | 2 | – | 2 | – | |
| Hirozane et al. (23) | 2015 | Case Report | 28 | – | 1 | – | 1 | |
| Hepp et al. (14) | 2019 | Case Report | 27 | – | 1 | 1 | – | |
| Rabelo et al. (24) | 2015 | Case Series | 27 | 2 | 3 | – | 5 | |
| Zitouna et al. (25) | 2018 | Case Report | 14 | 1 | – | – | 1 | |
| He et al. (26) | 2016 | Case Report | 10 | 1 | – | – | 1 | |
| Song et al. (28) | 2017 | Case Report | 30 | – | 1 | – | 1 | |
| Delgado González et al. (31) | 2021 | Case Report | 29 | 1 | – | – | 1 | |
| Bor et al. (30) | 2011 | Case Report | 32 | – | 1 | – | 1 | |
| Yuasa et al. (29) | 2015 | Case Report | 29 | – | 1 | – | 1 | |
| Romans et al. (42) | 2020 | Case Report | 29 | – | 1 | 1 | – | |
| Ornetti et al. (27) | 2008 | Case Report | 10 | – | 1 | – | 1 | |
| Sánchez Lázaro et al. (41) | 2014 | Case Report | 19 | 1 | – | – | 1 | |
| Yates et al. (32) | 2011 | Case Report | 20 | 1 | – | – | 1 | |
| Singh et al. (33) | 2014 | Case Report | 15 | 1 | – | 1 | – | |
| Rovira Martí et al. (40) | 2016 | Case Series | 12 | 3 | 2 | 3 | 2 | |
| Hashem et al. (39) | 2015 | Case Report | 26 | – | 1 | – | 1 | |
| Kundu et al. (34) | 2004 | Case Report | 29 | 1 | – | – | 1 | |
| Nakase et al. (35) | 2007 | Case Series | 34 | 3 | 2 | – | 5 | |
| Matar et al. (37) | 2014 | Case Report | 20 | – | 1 | 1 | – | |
| Berenguer et al. (36) | 2012 | Case Report | 22 | – | 1 | 1 | – | |
| Roth et al. (38) | 1976 | Case Report | 27 | – | 1 | – | 1 | |
mCMS, modified Coleman methodology score.
Among the studies there were 4 case series and 19 case reports. According to the mCMS evaluation, the mean score of the studies reached was 23 points (10–34 points) as in Table 1.
We reached a population of 36 patients, equally divided between males and females. All the cases collected in the selected articles considered patients affected by PYCD diagnosed at different ages. Only one-third of the study population was indeed pediatric, while two-third were adult age (Table 1).
Fractures rate, location, and treatment
We studied a total of 57 fractures secondary mainly to low energy trauma (91%, 52/57) (Table 2).
Table 2
| Ref. | Fracture rate | Location | Treatment | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Femur | Tibia | Other | Plate fixation | Intramedullary fixation | External fixation | Conservative | |||
| Mahmoudi et al. (22) | 1 | – | 1 | – | – | – | – | 1 | |
| Grewal et al. (19) | 5 | 4 | 1 | – | 2 | – | 2 | 1 | |
| Hirozane et al. (23) | 1 | – | – | Patella | – | – | – | 1 | |
| Hepp et al. (14) | 4 | – | 2 | Pelvis [2] | – | – | – | 4 | |
| Rabelo et al. (24) | 12 | 9 | 1 | Clavicula; ulna | 6 | – | – | 6 | |
| Zitouna et al. (25) | 1 | – | – | C2–C3 posterior arch | – | – | – | 1 | |
| He et al. (26) | 1 | – | – | Clavicula | – | – | – | 1 | |
| Song et al. (28) | 1 | 1 | – | – | – | 1 | – | – | |
| Delgado González et al. (31) | 1 | 1 | – | – | – | 1 | – | – | |
| Bor et al. (30) | 5 | 2 | 2 | Olecranon | – | 3 | – | 2 | |
| Yuasa et al. (29) | 1 | 1 | – | – | 1 | – | – | – | |
| Romans et al. (42) | 1 | 1 | – | – | 1 | – | – | – | |
| Ornetti et al. (27) | 1 | – | – | L3 pedicle | – | – | – | 1 | |
| Sánchez Lázaro et al. (41) | 2 | – | 2 | – | 2 | – | – | – | |
| Yates et al. (32) | 1 | 1 | – | – | 1 | – | – | – | |
| Singh et al. (33) | 1 | 1 | – | – | – | – | – | 1 | |
| Rovira Martí et al. (40) | 6 | 2 | 2 | Clavicula; radius | 2 | 1 | – | 6 | |
| Hashem et al. (39) | 1 | 1 | – | – | – | 1 | – | – | |
| Kundu et al. (34) | 1 | 1 | – | – | – | 1 | – | – | |
| Nakase et al. (35) | 6 | 3 | 3 | – | – | 1 | 5 | – | |
| Matar et al. (37) | 1 | 1 | – | – | 1 | – | – | – | |
| Berenguer et al. (36) | 1 | – | 1 | – | – | – | – | 1 | |
| Roth et al. (38) | 2 | 2 | – | – | 2 | – | – | – | |
| Total | 57 | 31 | 15 | 11 | 18 | 9 | 7 | 26 | |
Based on the data analyzed, fractures occurred mainly in long bones, often bilateral: 54% (31/57) and 26% (15/57) of cases were respectively femur and tibia fractures. As for the remaining affected districts: 1 patella fracture, 2 pelvis fractures, 3 clavicula fractures, 3 forearm fractures, and finally 2 spinal fractures as showed in Table 2. Regarding the 54% of femur fractures in question, 13% (4/31) occurred in the proximal femur, while the remaining 87% (27/31) were diaphyseal. All 4 proximal femur fracture cases were treated with open reduction and internal fixation with plate and screws.
The diaphyseal femur fractures were treated as follow: 15% (4/27) with external fixator, 48% (13/27) with plate and screws, 26% (7/27) with intramedullary nailing, and eventually 11% (3/27) were treated conservatively. As for tibia fractures were reported exclusively shaft fractures: 20% (3/15) were treated with external fixator, 13% (2/15) with plate and screws, 13% (2/15) with intramedullary nailing, and finally 53% (8/15) were treated conservatively.
Outcomes
Only 13 authors focused on fracture healing and bony union timescales. As far as reported, bony union was achieved at an average of 11 months after surgery/trauma (range, 3 to 36 months).
Eleven authors reported complications in their experience, in particular: refracture occurred in 19% of cases (11/57), pseudoarthrosis in 30% (17/57) and finally infections of the implanted devices occurred in 3% of cases (2/57) (Table 3).
Table 3
| Ref. | Bony union (months) | Complications | |||
|---|---|---|---|---|---|
| Refracture | Pseudoarthrosis | Infection | Other | ||
| Mahmoudi et al. (22) | – | – | – | – | – |
| Grewal et al. (19) | – | 4 | – | – | – |
| Hirozane et al. (23) | 15 | – | 4 | – | – |
| Hepp et al. (14) | – | – | 8 | – | – |
| Rabelo et al. (24) | 6 | – | 1 | – | – |
| Zitouna et al. (25) | – | – | – | – | – |
| He et al. (26) | – | – | – | – | – |
| Song et al. (28) | 4 | – | – | – | – |
| Delgado González et al. (31) | 6, 12 | – | – | – | – |
| Bor et al. (30) | 4 | 2 | – | – | – |
| Yuasa et al. (29) | 3 | 1 | – | – | 1* |
| Romans et al. (42) | 6 | – | – | – | – |
| Ornetti et al. (27) | – | – | 1 | – | – |
| Sánchez Lázaro et al. (41) | – | – | – | – | – |
| Yates et al. (32) | – | – | 1 | – | – |
| Singh et al. (33) | – | – | – | – | – |
| Rovira Martí et al. (40) | – | 2 | 1 | – | – |
| Hashem et al. (39) | 12 | – | – | 1 | – |
| Kundu et al. (34) | 3 | – | – | – | – |
| Nakase et al. (35) | 36, 6, 32, 29, 12 | 2 | 1 | 1 | – |
| Matar et al. (37) | – | – | – | – | – |
| Berenguer et al. (36) | – | – | – | – | – |
| Roth et al. (38) | 9 | – | – | – | – |
| Total | 11 | 11 | 17 | 2 | 1 |
*, avascular femoral head necrosis.
Discussion
PYCD is a rare genetic skeletal dysplasia characterized by a combination of specific features. The skeleton of these patients is characterized by dense bone with thick cortices because of the altered bone turnover typical of this disease (43). Nevertheless, despite the high density of the bone, the long bones are brittle such that minimal trauma can easily lead to fracture, often being “spontaneous” (19), and refractures. To date, by virtue of the rarity of this condition, the debate about the proper management of patients affected by PYCD is still open, especially when it comes to fractures. From the data we collected it seems clear that the surgical approach and the device are entirely at surgeon’s discretion (44). Despite the bone peculiar characteristics of this disease, some authors have preferred intramedullary nailing as being effective in preventing refracture, due to the permanent fixation and in obtaining physiological alignment (30,35). Despite the successful data emerged, Delgado González et al. (31) and Kundu et al. (34) described the difficulties encountered during nailing in their experience; among them the reaming of the medullary canal that resulted challenging sometimes even leading to breakage of the drills. Because of the narrow medullary, occasionally lacking (24), and the osteosclerotic bone the option of closed intramedullary nailing was discarded by many authors over time who have therefore planned an open reduction and internal fixation with plate osteosynthesis (42,45). Hashem et al. (39), for example, finding problematic to enter the canal despite the use of guide wires and reamers, rescheduled the second surgery as a plate fixation. Even this technique, however, was not without its difficulties. According to Yuasa et al. (29) the drilling, particularly in the femoral neck, was quite difficult. Similarly also Roth et al. found challenging the insertion of a four-flanged nail due to the sclerotic bone (38). Some authors have therefore tried to overcome this by frequently changing the drill-bit (39) and irrigating constantly with cold saline to reduce the effects of the heat generated (37).
The choice of conservative treatment is often controversial: while surgical difficulties due to altered bone quality tempt orthopedics to lean toward this option, this same choice imposes long periods of bed rest in patients with inherent difficulties in bone healing.
Fracture healing times were not made explicit in more than half of the papers under review and therefore, no conclusions could be drawn. Singh et al. (33) and similarly Mahmoudi et al. (22) have defined the consolidation times as “normal”, having thus found no differences in their experience compared with non-syndromic patients. On the contrary, most authors made explicit how recovery times are much longer and more troublesome; Nakase et al. have reported the longest healing time (35).
In terms of complications, it seems clear that the most frequent is pseudoarthrosis highly dependent on the intrinsically altered blastic and clastic functions according to Rabelo et al. (24).
An imbalance between an increase in bone formation and a reduction in bone resorption could explain the increase in skeletal fragility in this condition and thus the high rate of fractures and refractures (32). The treatment in case of refracture again strictly depends on the surgeons’ experience. These data highlight the importance of long-term follow-up in this population due to the high risk of refracture, along with the already high propensity for experiencing other fractures, and to the recurrent cases of pseudarthrosis. To date, significant records about the risk of postoperative infection rate in these patients are not available, however literature shows that patients with PYCD are more likely to develop osteomyelitis of the jaws after surgical procedure (46).
Our data show a low rate of infections related to bone fracture amounting to 3%. Nakase et al. (35) reported a deep infection occurred at the site of nail insertion 2 weeks after surgery for which debridement and irrigation were performed while the nail was not removed. Four weeks after surgery, Hashem et al.’s (39) patient presented with persistent drainage of a seropurulent fluid through a 2 cm dehiscence from which methicillin-resistant S. aureus (MRSA) was isolated. Initially it was treated with oral antibiotics with poor signs of improvement, so debridement and irrigation were performed again without removing the nail. Finally, a single case of necrosis of the femoral head after treatment of an atypical subtrochanteric femoral fracture was described by Yuasa et al. (29), treated with cementless total hip arthroplasty followed by fixation of the fracture with cable and plate system.
Six “impending fracture” cases have also been reported found as an occasional finding or because of persistent pain (28,29,31,34,38,39). All cases concerned the femur and preventive surgical treatment specular to the contralateral femur was performed in all but one case which was instead treated conservatively. In all cases treated surgically, the surgery was performed synchronously to the contralateral. One exception was a single case in which the patient refused the surgery at first. Thus, it seems clear that there is a unanimous opinion regarding the preventive treatment of the impending fractures typical of this condition.
The papers subject of the present literature review had several methodological issues, particularly when considering the procedure in assessing the outcomes. Furthermore, the study population was too small due to the fact that almost all the studies were case reports and therefore the patient’s follow-up was often too short. However, except a few articles, most studies reported in detail the surgical technique specifying even any difficulties encountered (Tables 2,3).
Limitations
The present study has plenty of limitations especially because of the type of articles subject of this Systematic Review. For this reason, the final conclusions deduced within the study are limited by the retrospective design, highly variable level of detail, and low level of evidence of the included studies.
Conclusions
This review shows that treatments such as intramedullary nailing or internal plate fixation, in addition to providing mechanical support and alignment, offer continuous support for the delayed bone healing and the high risk of refracture in PYCD. However, the surgeon’s expertise and the unique characteristics of the individual patient still seem to guide the treatment choice. To date, therefore, there are no standardized guidelines. The level of evidence in the included studies is low as expressed by the calculated mCMS value, mainly due to the heterogeneity of the included articles. Despite the rarity of this condition, further studies should be carried out to define the optimal surgical management not only of fractures, but also of the frequent cases of refracture. In addition, it might be useful to investigate whether in bone diseases, such as PYCD, arming the long bones preventively may have clinical significance in preventive fractures and thus improving the patient’s outcome.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the PRISMA reporting checklist. Available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-19/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://jxym.amegroups.com/article/view/10.21037/jxym-22-19/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- LeBlanc S, Savarirayan R. Pycnodysostosis. 2020. In: Adam MP, Ardinger HH, Pagon RA, et al. editors. GeneReviews® [Internet]. Seattle: University of Washington, 1993-2022.
- Arman A, Bereket A, Coker A, et al. Cathepsin K analysis in a pycnodysostosis cohort: demographic, genotypic and phenotypic features. Orphanet J Rare Dis 2014;9:60. [Crossref] [PubMed]
- Gelb BD, Shi GP, Chapman HA, et al. Pycnodysostosis, a lysosomal disease caused by cathepsin K deficiency. Science 1996;273:1236-8. [Crossref] [PubMed]
- Xue Y, Cai T, Shi S, et al. Clinical and animal research findings in pycnodysostosis and gene mutations of cathepsin K from 1996 to 2011. Orphanet J Rare Dis 2011;6:20. [Crossref] [PubMed]
- Zheng H, Zhang Z, He JW, et al. A novel mutation (R122Q) in the cathepsin K gene in a Chinese child with Pyknodysostosis. Gene 2013;521:176-9. [Crossref] [PubMed]
- Drake MT, Clarke BL, Oursler MJ, et al. Cathepsin K Inhibitors for Osteoporosis: Biology, Potential Clinical Utility, and Lessons Learned. Endocr Rev 2017;38:325-50. [Crossref] [PubMed]
- Stark Z, Savarirayan R. Osteopetrosis. Orphanet J Rare Dis 2009;4:5. [Crossref] [PubMed]
- Valdes-Flores M, Hidalgo-Bravo A, Casas-Avila L, et al. Molecular and clinical analysis in a series of patients with Pyknodysostosis reveals some uncommon phenotypic findings. Int J Clin Exp Med 2014;7:3915-23. [PubMed]
- Bizaoui V, Michot C, Baujat G, et al. Pycnodysostosis: Natural history and management guidelines from 27 French cases and a literature review. Clin Genet 2019;96:309-16. [Crossref] [PubMed]
- Otaify GA, Abdel-Hamid MS, Mehrez MI, et al. Genetic study of eight Egyptian patients with pycnodysostosis: identification of novel CTSK mutations and founder effect. Osteoporos Int 2018;29:1833-41. [Crossref] [PubMed]
- Appelman-Dijkstra NM, Papapoulos SE. From disease to treatment: from rare skeletal disorders to treatments for osteoporosis. Endocrine 2016;52:414-26. [Crossref] [PubMed]
- Caracas HP, Figueiredo PS, Mestrinho HD, et al. Pycnodysostosis with craniosynostosis: case report of the craniofacial and oral features. Clin Dysmorphol 2012;21:19-21. [Crossref] [PubMed]
- Khoja A, Fida M, Shaikh A. Pycnodysostosis with Special Emphasis on Dentofacial Characteristics. Case Rep Dent 2015;2015:817989. [Crossref] [PubMed]
- Hepp N, Frederiksen AL, Dunø M, et al. Multiple Fractures and Impaired Bone Fracture Healing in a Patient with Pycnodysostosis and Hypophosphatasia. Calcif Tissue Int 2019;105:681-6. [Crossref] [PubMed]
- Baglam T, Binnetoglu A, Fatih Topuz M, et al. Pycnodysostosis at otorhinolaryngology. Int J Pediatr Otorhinolaryngol 2017;95:91-6. [Crossref] [PubMed]
- Turan S. Current research on pycnodysostosis. Intractable Rare Dis Res 2014;3:91-3. [Crossref] [PubMed]
- Bertola D, Amaral C, Kim C, et al. Craniosynostosis in pycnodysostosis: broadening the spectrum of the cranial flat bone abnormalities. Am J Med Genet A 2010;152A:2599-603. [Crossref] [PubMed]
- Rothenbühler A, Piquard C, Gueorguieva I, et al. Near normalization of adult height and body proportions by growth hormone in pycnodysostosis. J Clin Endocrinol Metab 2010;95:2827-31. [Crossref] [PubMed]
- Grewal S, Kilic Ö, Savci-Heijink CD, et al. Disturbed remodeling and delayed fracture healing in pediatric pycnodysostosis patients. J Orthop 2019;16:373-7. [Crossref] [PubMed]
- Coleman BD, Khan KM, Maffulli N, et al. Studies of surgical outcome after patellar tendinopathy: clinical significance of methodological deficiencies and guidelines for future studies. Victorian Institute of Sport Tendon Study Group. Scand J Med Sci Sports 2000;10:2-11. [Crossref] [PubMed]
- Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Rev Esp Cardiol (Engl Ed) 2021;74:790-9. Erratum in: Rev Esp Cardiol (Engl Ed) 2022;75:192. [Crossref] [PubMed]
- Mahmoudi A, Bouabdallah Y. Pycnodysostosis presented with tibial shaft fracture. Pan Afr Med J 2020;35:5. [Crossref] [PubMed]
- Hirozane T, Suzuki T, Yoshida H. Pycnodysostosis with a patella fracture. Lancet Diabetes Endocrinol 2015;3:826. [Crossref] [PubMed]
- Rabelo FD, do Prado CH, Rabelo FL, et al. Reconsiderations regarding time of fracture healing in pycnodysostosis. Rev Bras Ortop 2015;45:606-11. [Crossref] [PubMed]
- Zitouna K, Jrad M, Miladi M, et al. Traumatic cervical spine injuries in a patient with pycnodysostosis. Eur J Orthop Surg Traumatol 2018;28:1231-3. [Crossref] [PubMed]
- He L, Winalski CS, Deal C, et al. Left clavicular fracture. Pyknodysostosis. Skeletal Radiol 2016;45:821-3, 851-2.
- Ornetti P, Prati C, Fery-Blanco C, et al. Pedicle stress fracture: an unusual complication of pycnodysostosis. Clin Rheumatol 2008;27:385-7. [Crossref] [PubMed]
- Song HK, Sohn YB, Choi YJ, et al. A case report of pycnodysostosis with atypical femur fracture diagnosed by next-generation sequencing of candidate genes. Medicine (Baltimore) 2017;96:e6367. [Crossref] [PubMed]
- Yuasa T, Maeda K, Kaneko K, et al. Total Hip Arthroplasty after Treatment of an Atypical Subtrochanteric Femoral Fracture in a Patient with Pycnodysostosis. Case Rep Orthop 2015;2015:731910. [Crossref] [PubMed]
- Bor N, Rubin G, Rozen N. Fracture management in pycnodysostosis: 27 years of follow-up. J Pediatr Orthop B 2011;20:97-101. [Crossref] [PubMed]
- Delgado González A, Morales Viaji JJ, López Díez ME. Bilateral subtrochanteric femoral fracture due to a very rare disease: Pycnodisostosis. Rev Esp Cir Ortop Traumatol (Engl Ed) 2021. [Epub ahead of print]. doi:
10.1016/j.recot.2021.01.005 .10.1016/j.recot.2021.01.005 - Yates CJ, Bartlett MJ, Ebeling PR. An atypical subtrochanteric femoral fracture from pycnodysostosis: a lesson from nature. J Bone Miner Res 2011;26:1377-9. [Crossref] [PubMed]
- Singh S, Sambandam B. A case of pycnodysostosis presented with pathological femoral shaft fracture. Indian J Med Res 2014;139:180-1. [PubMed]
- Kundu ZS, Marya KM, Devgan A, et al. Subtrochanteric fracture managed by intramedullary nail in a patient with pycnodysostosis. Joint Bone Spine 2004;71:154-6. [Crossref] [PubMed]
- Nakase T, Yasui N, Hiroshima K, et al. Surgical outcomes after treatment of fractures in femur and tibia in pycnodysostosis. Arch Orthop Trauma Surg 2007;127:161-5. [Crossref] [PubMed]
- Berenguer A, Freitas AP, Ferreira G, et al. A child with bone fractures and dysmorphic features: remember of pycnodysostosis and craniosynostosis. BMJ Case Rep 2012;2012:bcr2012006930. [Crossref] [PubMed]
- Matar HE, James LA. A challenging paediatric pathological femur fracture in pyknodysostosis (osteopetrosis acro-osteolytica): lessons learnt. BMJ Case Rep 2014;2014:bcr2014207730. [Crossref] [PubMed]
- Roth VG. Pycnodysostosis presenting with bilateral subtrachanteric fractures: case report. Clin Orthop Relat Res 1976;247-53. [PubMed]
- Hashem J, Krochak R, Culbertson MD, et al. Atypical femur fractures in a patient with pycnodysostosis: a case report. Osteoporos Int 2015;26:2209-12. [Crossref] [PubMed]
- Rovira Martí P, Ullot Font R. Orthopaedic disorders of pycnodysostosis: a report of five clinical cases. Int Orthop 2016;40:2221-31. [Crossref] [PubMed]
- Sánchez Lázaro JA, Linares Álvarez L. Pycnodysostosis: a rare disease with frequent fractures. Semergen 2014;40:e47-50. [PubMed]
- Romans M, Sambandam B, Moses J, et al. A rare case of pycnodysostosis: Technical difficulties in managing long bone fractures. J Clin Orthop Trauma 2020;11:332-8. [Crossref] [PubMed]
- Ketterer S, Gomez-Auli A, Hillebrand LE, et al. Inherited diseases caused by mutations in cathepsin protease genes. FEBS J 2017;284:1437-54. [Crossref] [PubMed]
- Vitiello R, Lillo M, Donati F, et al. Locking plate fixation in pediatric femur fracture: evaluation of the outcomes in our experience. Acta Biomed 2019;90:110-5. [PubMed]
- Gandhi GS, Vijayanarasimhan V, John L, et al. Fracture Management in Pyknodysostosis - A Rare Case Report. J Orthop Case Rep 2017;7:54-8. [PubMed]
- de França GM, Felix FA, de Morais EF, et al. Osteomyelitis of the jaws in patients with pycnodysostosis: a systematic review. Braz J Otorhinolaryngol 2021;87:620-8. [Crossref] [PubMed]
Cite this article as: Bocchi MB, Palmacci O, Bonfiglio N, Giuli C, Maccauro G, Vitiello R. Surgical treatment, complications and preventive surgery of fractures in pycnodysostosis: a systematic review. J Xiangya Med 2022;7:29.


