
Eight weeks exercise training program for runners with mild-to-moderate symptoms after COVID-19 infection: a case report
Introduction
On March 11st 2020, the World Health Organization (WHO) declared the coronavirus disease 2019 (COVID-19) outbreak as a global pandemic. In the course of this pandemic, several positive tests have been reported among recreational and professional runners, while most of them developed either mild or no symptoms. In an attempt to provide clinical recommendations for a safe return to sports activities after COVID-19 infection, a group of international experts have proposed a scientifically guided and stepwise approach for a safe resumption of sports activities (1).
The possible negative consequences of COVID-19 infection present challenges for clinicians and trainers caring for runners and preparing them to return to exercise (1,2). In a recent publication, Metzl et al. reported that each patient with COVID-19 is unique and there can be a wide variance of how each patient experiences the illness (2). They also proposed that every patient with COVID-19 recovers at a unique rate and at the moment there is not any algorithm to determine exactly a stepwise approach in order to return to exercise (2). Thus, there is a lack of scientific knowledge, surrounding exercise training programs in COVID-19 infected runners. This is why trainers are not having the appropriate information in order to guide their athletes in a safe manner.
What is the ideal intensity, duration and frequency of exercise training programs? What are the keys for a successful restart of exercise training program, in order to avoid training errors? What do they want to know? These are some questions which need to be answered. In this sense, the purpose of this paper is to present an individualized exercise training program for runners, who developed mild-to-moderate symptoms after COVID-19 infection. A secondary objective is to illustrate how medical guidance was made from the beginning of the infection to the final session of the exercise training program. We present the following case in accordance with the CARE reporting checklist (available at https://jxym.amegroups.com/article/view/10.21037/jxym-21-42/rc).
Case presentation
A 39-year-old male, who was a health care professional, with a body mass index of 23 kg/m2 and a past medical history of total thyroidectomy (over 15 years ago) due to follicular thyroid carcinoma, replaced with thyroxine (levothyroxime 137 mcg once daily), had been tested positive for COVID-19 (without symptoms) in the context of an employee monitoring in his workplace. As a result, he was recommended to be home quarantined, in order to prevent further transmission. His training status was an average of 30–35 km, 3 to 4 times per week for over 3 years. During the third day of his in-home self-isolation, the patient reported a sudden onset of symptoms with mild cough, headache, neck pain, fever (≤37.6 ℃), anosmia and ageusia. Standard treatment with paracetamol was used in order to relieve the symptoms and about 8 days later, he was revealed asymptomatic. Two weeks later, the decision to start exercise was based on the results of clinical examination by a sport physician.
A semi-structured interview was conducted with the patient to evaluate his training needs. Based on data from the interview, a frame-work was created in order to address his needs. A steering group was established to design the exercise training program, comprising by a sport physician, an exercise trainer and the runner. Aa a result, it was derived by the above team that the exercise training program should consist of two components: the medical and the training guidance.
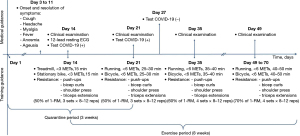
The final exercise training program was directly supervised by a specialized exercise trainer and consisted of endurance and resistance exercises, 5 days per week for 8 weeks. As a rule, training weeks had 2 days of rest or 1 more day according to the individuals’ need. The intensity and duration of exercise sessions were gradually increased during the exercise training program. A medical evaluation was usually performed by a sport physician before the increase of training intensity and duration. For the first week, the regular endurance exercises performed 2 to 3 times per week, the individual walked or/and biked on a motor driven treadmill and a stationary bike based on metabolic equivalents (METs). For the remaining 7 weeks of the exercise training program, treadmill and stationary bike were replaced with outdoor running and cycling (Figure 1). Meanwhile, the regular resistance exercises performed 2 times per week. Resistance exercises, with the use of free weights, targeted to the major upper body muscle groups (Figure 1). The one-repetition maximum (1-RM) test was used to assess the strength. The percentages chosen were 50%, 60%, and 70% of 1-RM. These particular moderate loading were recommended as they are the most commonly used in recreational athletes to maximize muscular strength. The classic periodization model on changing exercise intensity and duration was used, since it is commonly used in rehabilitation exercise protocols (3).
After 3 weeks of quarantine period and 8 weeks of supervised exercise training program, the runner was exercising without restrictions in the intensity and the duration of exercise and he did not report any further symptoms or exercise-related complaints. No pathological abnormalities were confirmed during the medical examination and the runner could regularly restart to participate in running events as previous. Six months after the initiation of intervention, the patient was contacted for the final follow-up. He reported that he has been running 5 to 10 km at least 4 times a week the last month and he has participated in a virtual race of 10 km without any complaint. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
It is well known that after a period of rest, due to a viral infection, physicians recommend the gradual return to exercise training, combined with monitoring of remaining symptoms of illness (4). Additionally, for athletes who have spent weeks at home recovering from a virus infection, it is of great importance to follow a well individualized exercise training program (5). Thus, an individualized exercise training program should be followed, avoiding prolonged and intense exercise, particularly during the first weeks of resumption of exercise. Prolonged exhaustive or high-intensity exercise causes immunosuppression and increases the risk of infection, while moderate exercise exerts less stress on the immune system and potentially reduces the risk and severity of respiratory viral infection (6). From a practical point of view, after a mild to moderate illness, return to exercise appears to be more beneficial if it starts with 1 week of light exercise, followed by gradually heavier exercise training program.
This particular case report showed the importance of a well individualized exercise training program and a comprehensive medical guidance. In this aspect, the individual was regularly evaluated by a sport physician and supervised by a specialized exercise trainer. The runner managed to successfully complete an 8-week exercise training program and was able to return to running events and in his previous sports level without any restrictions.
From the beginning of the declaration of the global pandemic, the international literature was enriched with practical guides and recommendations for a safe return to exercise (1,2,7). Individuals with COVID-19 infection experience a wide range of symptoms, ranging from being asymptomatic to severe illness (1). Hence, safe return to sports is another hot issue for the scientific community and requires the development of protocols (8). It is very important for the person to start training at an early stage after COVID-19 infection, although, early return to sports can lead to cardiovascular, respiratory and chronic muscle fatigue complications that may hinder exercise tolerance (2,8). Due to the fact that initial signs of physical and functional deconditioning are present from the first week (9), the gradual return of the exercise training is important, under the guidance of a multidisciplinary team (8).
Woods et al. stated that symptoms, such as fever, cough, shortness of breath and breathing difficulties, can appear within 2 to 14 days after infection and the athletes should seek medical diagnosis and discontinue physical activity and exercise immediately (10). It is important to note that during acute infection or in the recovery phase, high intensity exercise may result in overstrain, which can lead to immune system dilapidation and may be associated with the recurrence of COVID-19 infection (7,11). Additionally, it should be emphasized that recurrence or re-infection with COVID-19 could cause possible worse clinical outcomes and long-term complications (12).
Despite the multiple organ involvement in COVID-19, return to sports activity should be encouraged after overall recovery from acute respiratory infection. Moreover, due to the bed rest and long periods of deconditioning, athletes’ performance may be lost and as a result they have an increased risk of injury (7,13). To avoid all the negative consequences resulting from an early return to exercise and/or a non-well-designed exercise training programs, which is not tailored to athletes need; Barker-Davies et al. have proposed three METs for an initial period of approximately 2 weeks (6). An exercise training program must be initiated at low-intensity, while it could be gradually made more rigorous based on individual needs (14,15). It is unequivocal that each training program must be individualized in order to optimize the balance between strain and adaptation processes and of course to enhance athlete’s performance (7,13).
Conclusions
To summarize, the decision to restart sports activities, as well as running, should be a shared decision between healthcare professionals, sport physicians and exercise trainers. An individualized exercise training program, according to the runner’s needs, is very important and it can lead to favorable clinical outcomes, optimizing athletes’ performance. Finally, it should be noted that all the above guidelines are general and that acceptable levels of exercise initiation depend on the runner’s demands.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://jxym.amegroups.com/article/view/10.21037/jxym-21-42/rc
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at https://jxym.amegroups.com/article/view/10.21037/jxym-21-42/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Löllgen H, Bachl N, Papadopoulou T, et al. Infographic. Clinical recommendations for return to play during the COVID-19 pandemic. Br J Sports Med 2021;55:344-5. [Crossref] [PubMed]
- Metzl JD, McElheny K, Robinson JN, et al. Considerations for Return to Exercise Following Mild-to-Moderate COVID-19 in the Recreational Athlete. HSS J 2020;16:102-7. [Crossref] [PubMed]
- Lorenz D, Morrison S. Current concepts in periodization of strength and conditioning for the sports physical therapist. Int J Sports Phys Ther 2015;10:734-47. [PubMed]
- Börjesson M, Arvidsson D, Rensburg CJV, et al. Return to play after infectious disease. In: Musahl V, Karlsson J, Krutsch W, et al. editors. Return to Play in Football. Berlin, Heidelberg: Springer, 2018:755-69.
- Friman G, Wesslén L. Infections and exercise in high‐performance athletes. Immunol Cell Biol 2000;78:510-22. [Crossref] [PubMed]
- Barker-Davies RM, O'Sullivan O, Senaratne KPP, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med 2020;54:949-59. [Crossref] [PubMed]
- Vasiliadis AV, Boka V. Safe Return to Exercise after COVID-19 Infection. Sultan Qaboos Univ Med J 2021;21:373-7. [Crossref] [PubMed]
- Chiampas GT, Ibiebele AL. A Sports Practitioner's Perspective on the Return to Play During the Early Months of the COVID-19 Pandemic: Lessons Learned and Next Steps. Sports Med 2021;51:89-96. [Crossref] [PubMed]
- Clément G, Bareille MP, Goel R, et al. Effects of five days of bed rest with intermittent centrifugation on neurovestibular function. J Musculoskelet Neuronal Interact 2015;15:60-8. [PubMed]
- Woods JA, Hutchinson NT, Powers SK, et al. The COVID-19 pandemic and physical activity. Sports Med Health Sci 2020;2:55-64. [Crossref] [PubMed]
- Gousseff M, Penot P, Gallay L, et al. Clinical recurrences of COVID-19 symptoms after recovery: Viral relapse, reinfection or inflammatory rebound? J Infect 2020;81:816-46. [Crossref] [PubMed]
- Salcin S, Fontem F. Recurrent SARS-CoV-2 infection resulting in acute respiratory distress syndrome and development of pulmonary hypertension: A case report. Respir Med Case Rep 2021;33:101314. [Crossref] [PubMed]
- Halle M, Bloch W, Niess AM, et al. Exercise and sports after COVID-19-Guidance from a clinical perspective. Transl Sports Med 2021;4:310-8. [Crossref] [PubMed]
- González K, Fuentes J, Márquez JL. Physical Inactivity, Sedentary Behavior and Chronic Diseases. Korean J Fam Med 2017;38:111-5. [Crossref] [PubMed]
- Pate RR, Pratt M, Blair SN, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995;273:402-7. [Crossref] [PubMed]
Cite this article as: Vasiliadis AV, Boka V. Eight weeks exercise training program for runners with mild-to-moderate symptoms after COVID-19 infection: a case report. J Xiangya Med 2022;7:20.


