
Cardiac imaging findings of recovered COVID-19 patients with increased myocardial injury biomarkers in acute phase—the role of Multimodal cardiovascular imaging examination
There is no doubt that COVID-19 could cause cardiac injuries (1-7), and cardiovascular imaging examination including Cardiac Magnetic Resonance Imaging (CMR) and Coronary Computed Tomography Angiography (CCTA) are helpful for detecting cardiovascular injury and exploring pathophysiological mechanisms of multiple cardiovascular disease include COVID-19 (3-7). Chen et al. (4) performed CMR in 25 COVID-19 patients with at least one marker of cardiac involvement [cardiac symptoms, abnormal electrocardiograph (ECG), or abnormal cardiac biomarkers] within the first 10 days of the onset of COVID symptoms, and found in patients with early-stage COVID-19, myocardial edema, and functional abnormalities are a frequent finding, while irreversible regional injury such as necrosis may be infrequent. However, considering the risk of infection associated with patient transport and imaging examination, it is not feasible to learn cardiovascular injury by multiple imaging examinations during the acute phase in most hospitals.
To provide imaging evidence and basis for revealing the pathogenesis of myocardial injury of COVID-19, CMR and CCTA were performed on recovered COVID-19 patients whose virus detection turned negative and clinical observation was done in our hospital prospectively. The selection criterions were as follows: (I) patients were previously confirmed of SARS-CoV-2 infection by reverse transcription and polymerase chain reaction (RT-PCR) swab test; (II) patients were considered recovered by the discharging criteria (a. normal temperature lasting longer than 3 days; b. resolved respiratory symptoms; c. substantially improved acute exudative lesions on chest CT images; d. two consecutive negative RT-PCR test results separated by at least 24 hours and was isolated for 14 days; (III) the recovery of respiratory function and being able to tolerate the special respiration requirements of CMR. This study was approved by the institutional review board of the Fifth Affiliated Hospital of Sun Yat-sen university (No.: K214-1).
Seven COVID-19 patients who recently recovered from COVID-19 infection were included. Patient characteristics, blood test results, treatment before discharge and CMR imaging findings are provided in Table 1.
Table 1
| Characteristics | Cases | |||||||
|---|---|---|---|---|---|---|---|---|
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | ||
| Patient characteristics | ||||||||
| Gender | F | F | F | M | F | M | M | |
| Age (years) | 75 | 70 | 59 | 38 | 22 | 29 | 36 | |
| BMI | 23.22 | 31.25 | 26.2 | 22.25 | 15.6 | 21.25 | 24.9 | |
| Comorbidities | ||||||||
| Hypertension | Y | Y | N | N | N | N | N | |
| Diabetes mellites | N | N | N | N | N | N | N | |
| Known Coronary artery disease | N | N | N | N | N | N | N | |
| Chronic obstructive pulmonary diseases | N | N | N | N | N | N | N | |
| Cerebrovascular disease | N | Y | N | N | N | N | N | |
| Chronic renal diseases | N | N | N | N | N | N | N | |
| Chronic liver diseases | N | N | N | N | N | N | N | |
| Blood pressure, mmHg | ||||||||
| Systolic | 174 | 130 | 154 | 108 | 108 | 125 | 118 | |
| Diastolic | 86 | 62 | 94 | 76 | 72 | 87 | 79 | |
| Heart rate (highest), beats per min | 85 | 71 | 67 | 86 | 70 | 72 | 94 | |
| Duration between confirming of COVID-19 to CMR examination (day) | 54 | 59 | 27 | 48 | 51 | 43 | 54 | |
| Clinical types | Critical | Severe | Common | Severe | Common | Mild | Severe | |
| Precordial chest pain | Acute | N | N | N | N | N | N | N |
| Convalescents | N | N | N | N | N | N | N | |
| Palpitation | Acute | N | N | N | N | N | N | N |
| convalescents | Y | N | Y | N | N | N | N | |
| Chest distress | Acute | Y | N | N | Y | Y | Y | N |
| Convalescents | Y | N | Y | N | N | N | N | |
| Blood test results | ||||||||
| Laboratory findings | NRR | |||||||
| White blood cell count (×109/L) | 3.5–9.5 | 21.24h | 10.25h | 4.43h | 5.91h | 5.14h | 7.45h | 12.2h |
| 3.79L | 3.85L | 2.53L | 2.47L | 2.21L | 4.92L | 4.45L | ||
| Lymphocyte count (×109/L) | 1.1–3.2 | 0.97h | 1.56h | 1.14h | 1.56h | 1.48h | 2.46h | 1.71h |
| 0.31L | 0.54L | 0.84L | 0.64L | 0.89L | 1.43L | 0.68L | ||
| Platelet count (×103/L) | 152–350 | 345h | 182h | 189h | 274h | 370h | 269h | 373h |
| 304L | 117L | 163L | 118L | 201L | 232L | 142L | ||
| Red blood cell count (×109/L) | 3.8–5.1 | 3.75h | 3.52h | 4.05h | 5.48h | 4.42h | 5.55h | 4.77h |
| 3.04L | 3.05L | 3.65L | 4.53L | 3.43L | 5.08L | 4.17L | ||
| Hemoglobin, g/L | 115–150 | 109h | 112h | 127h | 162h | 138h | 169h | 149h |
| 85L | 92L | 117L | 131L | 108L | 154L | 133L | ||
| Procalcitonin, ng/mL | 0–0.5 | 1.24h | 0.26h | 0.11h | 0.17h | 0.48h | 0.13h | 0.16h |
| 0.12L | <0.10L | <0.10L | <0.10L | <0.10L | <0.10L | <0.10L | ||
| CRP (highest) (mg/L) | 0.068–8.2 | 127.5h | 45.79h | 0.460h | 19.52h | 5.590h | 0.210h | 46.57h |
| 12.9L | 1.22L | <0.220L | 0.560L | <0.120L | >0.03L | 3.19L | ||
| Hs-cTnI (pg/mL) | 0–0.0229 | 0.15h | 0.056h | <0.010h | 0.017h | <0.010h | <0.010h | <0.010h |
| <0.010L | <0.010L | <0.010L | <0.010L | <0.010L | <0.010L | <0.010L | ||
| Creatinine kinase–myocardial band, U/L | 0–25 | 10.7h | 15h | 30.7h | 34.9h | 25.9h | 26.8h | 29.30h |
| Glutamic Oxaloacetic Transaminase, U/L | 13–35 | 117h | 80.10h | 21.5h | 29h | 28.2h | 19.3h | 36.8h |
| Glyoxylate Aminotransferase, U/L | 7–40 | 55.1h | 100.8h | 14.4h | 25.2h | 32.2h | 13.0h | 63.1h |
| Albumin, g/L | 40–55 | 30.2L | 32.3L | 36.5L | 33.6L | 37L | 40.3L | 44.1L |
| Myoglobin, μg/L | 23–112 | / | / | 29 | / | 31 | / | / |
| NT-proBNP, μg/L | 0–125 | 4,480h | 4,710h | 156h | 123h | 53h | 20h | 932h |
| 149L | 496L | 80L | 51L | <20L | 20L | <20L | ||
| DD-dimer (ng/mL) | 0–243 | 1,087h | 491h | 2,093h | 284h | 109h | 61h | 423h |
| 208L | 121L | 40L | 89L | 57L | 23L | 252L | ||
| Arterial oxygen saturation | 0.93–0.98 | 0.622L | 0.89L | 0.981L | 0.952L | 0.982L | 0.92L | 0.959L |
| 0.988h | 1.003h | 1.001h | 0.999h | 1.005h | 0.989h | 0.994h | ||
| Revised arterial oxygen partial pressures | 83-108 | 39.6L | 56.7L | 87.1L | 38.6L | 101L | 87.2L | 77.20L |
| Creatinine, μmol/L | 41-81 | 89.4h | 75.2h | 71.5h | 105h | 81h | 75.6h | 106h |
| Treatment before discharge | ||||||||
| Antiviral therapy | Y | Y | Y | Y | Y | Y | Y | |
| Antibiotic therapy | Y | Y | Y | Y | Y | N | Y | |
| Intensive immunotherapy | Y | Y | Y | Y | Y | Y | Y | |
| Hydroxychloroquine | N | N | Y | Y | Y | N | Y | |
| Use of corticosteroid | Y | N | N | N | N | N | Y | |
| Nasal cannula oxygen | Y | Y | N | Y | Y | N | Y | |
| Non-invasive ventilation or high-flow nasal cannula oxygen | Y | Y | N | N | N | N | N | |
| CMR findings | ||||||||
| LV function | ||||||||
| ED Mass/BSA (g/m2) | 56.19 | 93.61 | 52.97 | 52.46 | 41.75 | 60.02 | 56.34 | |
| EDV/BSA (mL/m2) | 42.28 | 97.61 | 66.45 | 88.54 | 68.24 | 74.97 | 61.38 | |
| ESV/BSA (mL/m2) | 14.07 | 48.75 | 39.1 | 36.7 | 25.17 | 29.19 | 21.83 | |
| SV/BSA (mL/m2) | 28.21 | 48.86 | 27.35 | 51.84 | 43.08 | 45.78 | 39.55 | |
| CI (L/min/m2) | 2.48 | 3.18 | 1.64 | 2.64 | 3.88 | 3.25 | 3.01 | |
| LVEF, % | 75.92 | 50.05 | 41.15 | 58.55 | 63.12 | 61.06 | 64.44 | |
| RV function | ||||||||
| EDV/BSA (mL/m2) | 55.66 | 38.56 | 60.79 | 70.44 | 61.78 | 81.4 | 64.51 | |
| ESV/BSA (mL/m2) | 17.43 | 15.8 | 34.03 | 33.87 | 30 | 41.46 | 32.14 | |
| SV/BSA (mL/m2) | 38.23 | 22.77 | 26.77 | 36.57 | 31.78 | 39.94 | 32.37 | |
| RVEF | 68.68 | 59.04 | 44.03 | 51.91 | 51.44 | 49.06 | 50.18 | |
| CI (L/min/m2) | 3.62 | 1.48 | 1.61 | 1.8 | 2.86 | 2.91 | 2.46 | |
| LGE (%) | 2.96 | 8.78 | 5.23 | 4.51 | 0.61 | 0.84 | 0 | |
| Ischemic | Y | Y | N | N | N | N | / | |
| Nonischemic | Y | N | Y | Y | Y | Y | / | |
| Edema | N | Y | N | N | N | N | N | |
| Pericardial | N | N | N | N | N | N | N | |
| Pericardial effusion | N | N | N | N | N | N | N | |
Six (85.71%) patients were found of myocardial injury. The final diagnosis are: Case 1: hypertensive cardiomyopathy, coronary artery disease (CAD), coronary artery fistula, ischemic injury of left ventricular basal lateral wall and myocarditis of left ventricular basal inferior and septal wall caused by Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) infection (Figure 1); Case 2: CAD, chronic total occlusion (CTO) of LAD and LCX, ischemic cardiomyopathy, left ventricular aneurysm, CAD induced ischemic myocardial injury under the condition of ischemia and hypoxia of COVID-19 (Figure 2); Case 3, 4, 5, 6: myocarditis caused by SARS-CoV-2 infection (Figure 3); CMR of Case 7 was negative.
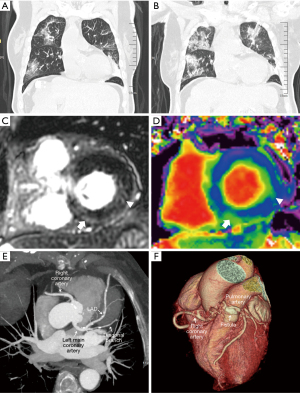
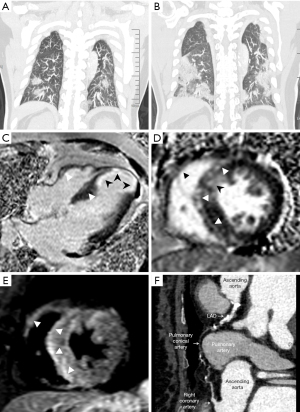
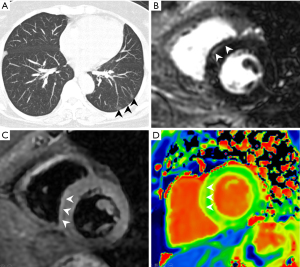
Most studies of cardiovascular imaging in recovered COVID-19 patients used CMR only (3,5-7), myocardial edema, fibrosis, and impaired ventricular function are common, however the cause were not discussed by direct imaging evidence. We performed CMR and CCTA on patients 1 and 2 simultaneously, which make it possible to find out the cause. Our results show myocardial injury of COVID-19 patients persistent until early convalescent stage, and maybe caused by multiple factors, including myocarditis, ischemic injury caused by the condition of ischemia and hypoxia of COVID-19, they may occur at the same time and serious injury was more likely to occur in patients with a history of cardiovascular disease. Cardiovascular imaging examination including CMR and CCTA are helpful to confirm it and find out the cause.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://dx.doi.org/10.21037/jxym-21-23). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020;395:497-506. [Crossref] [PubMed]
- Wu Z, McGoogan JM. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239-42. [Crossref] [PubMed]
- Wang H, Li R, Zhou Z, et al. Cardiac involvement in COVID-19 patients: mid-term follow up by cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2021;23:14. [Crossref] [PubMed]
- Chen BH, Shi NN, Wu CW, et al. Early cardiac involvement in patients with acute COVID-19 infection identified by multiparametric cardiovascular magnetic resonance imaging. Eur Heart J Cardiovasc Imaging 2021;22:844-51. [Crossref] [PubMed]
- Huang L, Zhao P, Tang D, et al. Cardiac Involvement in Patients Recovered From COVID-2019 Identified Using Magnetic Resonance Imaging. JACC Cardiovasc Imaging 2020;13:2330-9. [Crossref] [PubMed]
- Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol 2020;5:1265-73. [Crossref] [PubMed]
- Pan C, Zhang Z, Luo L, et al. Cardiac T1 and T2 Mapping Showed Myocardial Involvement in Recovered COVID-19 Patients Initially Considered Devoid of Cardiac Damage. J Magn Reson Imaging 2021;54:421-8. [Crossref] [PubMed]
Cite this article as: Pan C, Luo L, Qin P, Ye Y, Ding X, Wu W, Zhang Z, Chen J, Li S. Cardiac imaging findings of recovered COVID-19 patients with increased myocardial injury biomarkers in acute phase—the role of Multimodal cardiovascular imaging examination. J Xiangya Med 2021;6:26.


