
Atrial flutter with 1:1 rapid wide QRS atrioventricular conduction in a patient following traditional surgical repair on atrial septal defect: a case study
Introduction
A patient developed atrial flutter (AFL) with 1:1 rapid wide QRS atrioventricular conduction (AVC). The patient underwent a traditional pericardial patch technique for the atrial septal defect 2 years ago. Her electrocardiogram (ECG) during the arrhythmia attack revealed wide QRS tachycardia with rates of 250 beats per minute. AFL with 1:1 wide QRS tachycardia may present a clinical diagnostic challenge. AFL with 1:1 AVC must be differentiated from rapid arrhythmias, such as ectopic atrial tachycardia (AT), AV node reentrant tachycardia (AVNRT), and ventricular tachycardia (VT). We did Brugada’s stepwise approach and the VT score for the diagnosis. Meanwhile, we did RS/QRS ratio in lead V6. Amiodarone was administered under the guidance of a cardiovascular physician. Through observations of the dynamic changes during and after amiodarone treatment, we made the diagnosis. It is crucial to avoid mismanagement/misdiagnosis in patients with wide QRS complex tachycardia and rates above 200 beats per minute. We present the following case report in accordance with the CARE reporting checklist (available at http://dx.doi.org/10.21037/jxym-21-4).
Case presentation
Clinical data
A 54-year-old female who had experienced choledochotomy and cholecystectomy for Choledocholithiasis and cholecystolithiasis went to the emergency department at 14:33 on July 16, 2020. Our case complied with the Declaration of Helsinki and was approved by our local research ethics committees of the first affiliated hospital of the university of science and technology of China, with the patient giving written informed consent.
Past history
She had undergone tricuspid valve plasty for nonrheumatic tricuspid valve insufficiency and pericardial patch technique for the congenital atrial septal defect in 2018. She was with no history of hypertension and diabetes mellitus. She was without hepatitis and tuberculosis.
Personal history
She has no history of smoking or drinking.
Course of analysis
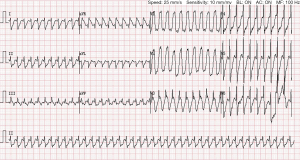
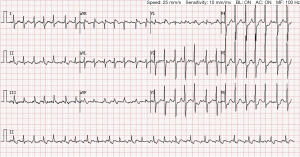
Her blood pressure at presentation was 109/75 mmHg, heart rate 96 bpm, afebrile, oxygen saturation (SaO2 99%). Cardiac rhythm is regular with no murmur. Her bedside ECG showed sinus rhythm (Figure 1). We performed a complete echocardiographic examination identifying the patient with left ventricular ejection fraction (EF) about 64%, tricuspid valvuloplasty, and no shunt following repair of the atrial septal defect. One hospital day 2, blood routine analysis showed red blood cell (RBC) count 2.58×1012/L, hemoglobin 90.0 g/L, platelet count 112×109/L. Biochemistry test results revealed aspartic acid aminotransferase 53 U/L, total bilirubin 102.8 µmol/L, direct bilirubin 75.4 µmol/L. She was treated with inhibition of gastric acid secretion and rehydration. CT of the upper abdomen showed postoperative changes of the biliary tract and intrahepatic bile duct dilatation. On day 12 (July 28, 2020), the patient underwent percutaneous transhepatic biliary drainage. Postoperative reexamination of blood routine showed white blood cell count 11.29×109/L, RBC count 2.66×1012/L, hemoglobin 91.0 g/L, platelet count 105×109/L. On day 17 (August 2, 2020), 17:55, the patient occurred fever and chills. 19:00 her body temperature 41 °C, heart rate 250 bpm, with confusion and convulsion. ECG showed AFL with 1:1 wide QRS AVC (Figure 2). Diazepam was given 5 mg intravenously. One hundred and fifty mg amiodarone was given intravenously, following intravenous infusion 300 mg amiodarone. The patient was treated with Moxifloxacin antibiotic therapy. 20:34 ECG showed AFL with 2:1 AVC (Figure 3). Her blood pressure at presentation was 96/62 mmHg, heart rate 127 bpm. Her vital signs were stable without discomfort complaints. Finally, she was discharged from the department on August 21, 2020.
Discussion
We report a case of AFL with 1:1 rapid AVC in a cured congenital atrial septal defect. Initially, we did not immediately diagnosis this tachyarrhythmia due to the lack of intracardiac monitoring. We calculated the VT score, and the result showed score 1. Then we made Brugada’s stepwise approach to exclude the VT. Meanwhile, we did RS/QRS ratio in lead V6, and the result showed the rate of 0.369 (<0.41, cut off 0.41). The result also suggested that the wide QRS AV tachycardia was not VT. The cardiovascular physician gave the patient amiodarone. Amiodarone is a benzofuran derivative. The primary direct electrophysiologic effect of amiodarone on cardiac tissues and fibers is to prolong the refractoriness and repolarization. These tissues and fibers contained the sinus node (SN), atrium, AV node (AVN), His-Purkinje system, and ventricle. Through observations of the dynamic changes during and after amiodarone treatment, the third ECG, which was obtained more than 2 hours after the second ECG, obviously displayed AFL with 2:1 AVC. The rate of the AFL waves was identical to the rate of rapid arrhythmia attack. Retrospectively, the rapid arrhythmia electrocardiography was diagnosed as AFL with 1:1 AVC.
ASD is the third most common kind of congenital heart disease, with an estimated 56 per 100,000 live births. Surgical closure is safe and effective. It has been postulated that after repair of the ASD, survival is good, but pulmonary hypertension, SN dysfunction, atrial fibrillation, and flutter are mentioned as sequelae. So, we should consider the patient’s underlying heart disease to make a diagnosis of arrhythmia. AFL with 1:1 rapid wide QRS AVC has rarely been reported in the cardiovascular literature. AFL with 1:1 rapid AVC is considered one of the most life-threatening arrhythmias and hemodynamically perilous. The initial management and diagnosis of patients with AFL with 1:1 rapid wide QRS AVC is still a challenge. AFL with 1:1 AVC must be differentiated from ectopic AT, AVNRT, and VT (1). AFL is characterized by the ordered periodic atrial rhythm at an average rate of 200 to 400 beats min. There are generally no isoelectric segments between the periodically shaped, regular, biphasic saw-tooth. Although the rates of these tachycardias do not generally exceed 200 beats per minute, there are always few exceptions. 1:1 atrial ventricular conduction has been reported in patients who took sodium channel blockers. These drugs such as flecainide, quinidine, procainamide, and disopyramide slowed both the atrial conduction and the AFL rate itself (2-4). Recently, Class I antiarrhythmic drugs are less likely to be applied in clinical practice to convert AFL to sinus rhythm. For this reason, the drug-induced AFL with 1:1 AVC, which was once a common sight, is becoming rare. In a recent clinical report, Jessie pointed out a clinical case of AFL with 1:1 rapid AVC in Wolff-Parkinson-White syndrome (5). 1:1 atrial ventricular conduction might also be triggered by sympathetic stimulation (e.g., excitement, exercise, induction of anesthesia). It has been reported to happen spontaneously (6-10). Electrophysiologists recommend the radiofrequency ablation of the AFL circuit for therapy of AFL and 1:1 AVC. In contrast, neither the ablation of AVC nor the insertion of a permanent pacemaker is the optimized selection.
In conclusion, AFL with rapid 1:1 AVC is an uncommon happening but challenging and fatal arrhythmia. We should take into account the patient’s underlying heart disease to make a diagnosis of arrhythmia. Brugada’s stepwise approach and the VT score can assist clinical physicians in making the diagnosis. Our study also verifies the RS/QRS ratio in lead V6 is vital to differentiate supraventricular tachycardia (SVT) with a right bundle branch block (RBBB) pattern from VT. Through observation of the changes of ECG before and after amiodarone, we can make the diagnosis. It is crucial to be conscious of AFL's differential diagnosis with rapid wide QRS 1:1 AVC to avoid misdiagnosis and mismanagement.
Acknowledgments
I would like to thank Professor Liu Xian (Department of Cardiology, The Fourth Affiliated Hospital of Harbin Medical university) for her assisting as the language checker.
Funding: This study was supported by the Natural Science Foundation of Anhui Province of China (178085MH227).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jxym-21-4
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-21-4). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hegde S, Kumar V. Wide complex tachycardia in a patient with a history of atrial fibrillation. JAMA Intern Med 2016;176:386-8. [Crossref] [PubMed]
- Bhardwaj B, Lazzara R, Stavrakis S. Wide complex tachycardia in the presence of class I antiarrhythmic agents: a diagnostic challenge. Ann Noninvasive Electrocardiol 2014;19:289-92. [Crossref] [PubMed]
- Brembilla-Perrot B, Houriez P, Beurrier D, et al. Predictors of atrial flutter with 1:1 conduction in patients treated with class I antiarrhythmic drugs for atrial tachyarrhythmias. Int J Cardiol 2001;80:7-15. [Crossref] [PubMed]
- Taylor R, Gandhi MM, Lloyd G. Tachycardia due to atrial flutter with rapid 1:1 conduction following treatment of atrial fibrillation with flecainide. BMJ 2010;340:b4684. [Crossref] [PubMed]
- Nelson JG, Zhu DW. Atrial flutter with 1:1 conduction in undiagnosed Wolff-Parkinson-White syndrome. J Emerg Med 2014;46:e135-40. [Crossref] [PubMed]
- Kawabata M, Hirao K, Higuchi K, et al. Clinical and electrophysiological characteristics of patients having atrial flutter with 1:1 atrioventricular conduction. Europace 2008;10:284-8. [Crossref] [PubMed]
- Sud M, Wellens HJ, Jassal DS, et al. Dilated cardiomyopathy: an unexpected complication of rapidly conducted atrial flutter in the Wolff-Parkinson-White syndrome. Can J Cardiol 2012;28:119.e5-7. [Crossref] [PubMed]
- Turitto G, Akhrass P, Leonardi M, et al. Atrial flutter with spontaneous 1:1 atrioventricular conduction in adults: an uncommon but frequently missed cause for syncope/presyncope. Pacing Clin Electrophysiol 2009;32:82-90. [Crossref] [PubMed]
- Jastrzebski M, Sasaki K, Kukla P, et al. The ventricular tachycardia score: a novel approach to electrocardiographic diagnosis of ventricular tachycardia. Europace 2016;18:578-84. [Crossref] [PubMed]
- Kim M, Kwon CH, Lee JH, et al. Right bundle branch block-type wide QRS complex tachycardia with a reversed R/S complex in lead V6: Development and validation of electrocardiographic differentiation criteria. Heart Rhythm 2021;18:181-8. [Crossref] [PubMed]
Cite this article as: Li J, Wang Y, Zhang F, Gao M, Li X, Wang J, Di X, Wang M, Qiu X, Ding B. Atrial flutter with 1:1 rapid wide QRS atrioventricular conduction in a patient following traditional surgical repair on atrial septal defect: a case study. J Xiangya Med 2021;6:18.



