
IVUS-guided DK-crush left anterior descending-diagonal complex bifurcation PCI via redo distal transradial access
A bifurcation lesion is a coronary artery narrowing adjacent to and/or involving the origin of a significant side branch (SB) that should not be lost (1). Percutaneous coronary interventions (PCIs) involving bifurcation lesions are encountered in 15-20% of cases in daily practice (2). The inherent difficulty of bifurcation PCI stems from the fact that stent implantation in main branch (MB) may lead to acute impairment of flow in SB (3). With the double kissing-crush (DK-crush) technique, SB stent is deployed first, then crushed with a balloon in the MB, rewired, preferably by a central re-crossing, so first kissing balloon inflation (KBI) is performed. A second stent is deployed into the MB and the procedure is ideally finished with proximal optimization technique (POT), followed by second KBI and final POT (2,3). Seven Fr guiding catheters may be preferred when complex two-stent strategies are planned (3). In cases of increased procedure complexity (e.g., double stenting), intravascular ultrasound (IVUS) may offer additional information, including pre- and postprocedure evaluations of vessels and stents (2,3).
The adoption by our cath lab team of distal transradial access (dTRA) as default approach for coronary angiography (CAG) and interventions was recently published by Oliveira et al. (4). As a refinement of the conventional (proximal) TRA, this technique has many advantages in terms of patient and operator comfort, faster hemostasis and risk of radial artery occlusion (4).
A 70-year-old man with chest pain at minimal efforts and a high-risk treadmill test was referred by the assistant cardiologist to CAG, performed via right dTRA (rdTRA) 6 Fr, showing severe and calcified ostial-proximal left anterior descending (LAD) coronary stenosis, involving the bifurcation with an important first diagonal (D1) branch (Videos 1-3), also with severe ostial-proximal stenosis (Medina 1,1,1). There was yet an ambiguous mid circumflex narrowing, with preserved rest left ventricular contraction.
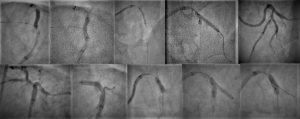
After consensual decision by the patient and the heart team, it was decided to perform IVUS-guided DK-crush LAD-D1 complex bifurcation PCI. Two days after the baseline CAG, the intended procedure was done via redo rdTRA, with a 7-Fr sheath (Figure 1). Baseline IVUS of LAD and D1 (Videos 4,5) evidenced fibrocalcific atheroma causing severe narrowings at both vessels. After predilations of D1 and LAD with a 2.5/20 mm non-compliant (NC) balloon, a 3/23 mm drug-eluting stent (DES) was carefully and optimally deployed at D1 ostial-proximal portion (Figure 2), after what the stent balloon was slightly withdrawn for subsequent high-pressure inflation (to flare proximal stent). By confirming no distal stent edge dissection, SB wire was completely removed and SB stent crushed with a MB 3/20 mm NC balloon (Figure 2). Then SB was rewired for first KBI—NC 4/8 mm (LAD) and NC 3/20 mm (D1)—Figure 2. A 3.5/28 mm DES was then carefully and optimally deployed at LAD ostial-proximal portion, involving LAD-D1 bifurcation, with only MB wired (Figure 2). POT was performed with a 4/8 mm NC balloon up to 26 atm (Figure 2). SB was again rewired for second KBI—NC 4/8 mm (LAD) and NC 3/20 mm (D1)—Figure 2. Final POT was repeated (Figure 2). IVUS runs of D1 and LAD (Videos 6,7) confirmed adequate stents expansion, apposition and symmetry, without edge dissections, fractures or geographic misses. A significant mid LAD myocardial bridging, starting just at distal stent edge, was highlighted by CAG (Videos 8-10) and IVUS (Video 7).

Adequate hemostasis was completely obtained after 2 hours with TR band device (Terumo Corp., Tokyo, Japan), without any bleeding. Proximal and distal right radial pulses were easily palpable after hemostasis and at hospital discharge, the morning day after, without any minor or major access site-related or clinical complications.
Complex bifurcation lesions requiring laborious DK-crush technique PCI with IVUS guidance can be safely and successfully performed via dTRA by experienced transradial operators, with patient and operator comfort and significant reduction of access site-related complications.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-20-58). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Louvard Y, Medina A. Definitions and classifications of bifurcation lesions and treatment. EuroIntervention 2015;11 Suppl V:V23-6.
- Banning AP, Lassen JF, Burzotta F, et al. Percutaneous coronary intervention for obstructive bifurcation lesions: the 14th consensus document from the European Bifurcation Club. EuroIntervention 2019;15:90-8. [Crossref] [PubMed]
- Milasinovic D, Wijns W, Ntsekhe M, et al. Step-by-step manual for planning and performing bifurcation PCI: a resource-tailored approach. EuroIntervention 2018;13:e1804-11. [Crossref] [PubMed]
- Oliveira MDP, Navarro EC, Kiemeneij F. Distal transradial access as default approach for coronary angiography and interventions. Cardiovasc Diagn Ther 2019;9:513-9. [Crossref] [PubMed]
Cite this article as: Oliveira MDP, Navarro EC, Caixeta A. IVUS-guided DK-crush left anterior descending-diagonal complex bifurcation PCI via redo distal transradial access. J Xiangya Med 2020;5:20.


