
Per-oral endoscopic myotomy after previous interventions for achalasia
Introduction
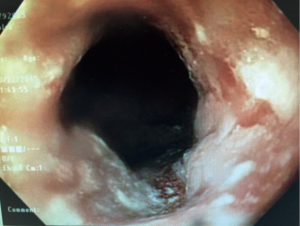
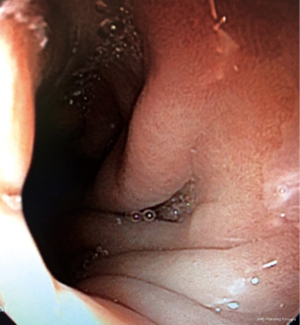
Per-oral endoscopic myotomy (POEM) for achalasia was first reported by Inoue et al. in 2010 (1). The concept of operating endoscopically in the wall of the esophagus was conceptualized by Pasricha et al. when seeking a way to perform natural orifice surgery (2). POEM rapidly became popular as a minimally invasive endoscopic technique by which to reduce high pressures of the lower esophageal sphincter in achalasia. Numerous reports have demonstrated the success of the method in the primary treatment of achalasia. Comparison with Heller myotomy, performed laparoscopically, have been favorable although most studies show a higher rate of postoperative gastroesophageal reflux after POEM (3). In recent years, a partial fundoplication is usually performed with a Heller myotomy in order to reduce postoperative reflux. Laparoscopic Heller myotomy is safe and extremely effective in the treatment of achalasia with reported success rates, based upon Eckardt scores, in excess of 90% (4). Occasionally however, patients are encountered in whom symptoms of dysphagia have returned or persisted. Such may also be the case after pneumatic dilation which is also effective in the treatment of achalasia. These patients must be carefully re-evaluated with endoscopy, esophageal manometry, and barium esophagram. In some cases, the problem may be something other than achalasia such as peptic stricture secondary to reflux or pseudoachalasia caused by a neoplasm (Figure 1). In still other instances the recurrent dysphagia may be due to progression of the underlying disease with mega esophagus and poor emptying in spite of a widely patent lower esophageal sphincter (Figure 2). In those patients where re-evaluation clearly defines delayed esophageal emptying secondary to high lower esophageal sphincter pressures and failure of relaxation, repeat surgery may be considered. Repeat Heller myotomy has been performed in such cases and is often effective. It must be performed in a lateral or posterior position which may occasionally be challenging. POEM is ideal in re-operative cases (5). The exact position and length of the myotomy can be specifically chosen. When recurrent symptoms occur after previous POEM, re-do POEM is still a good option. POEM after failed pneumatic dilation for achalasia has also been effective.
Technique
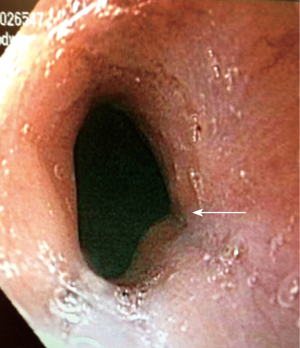
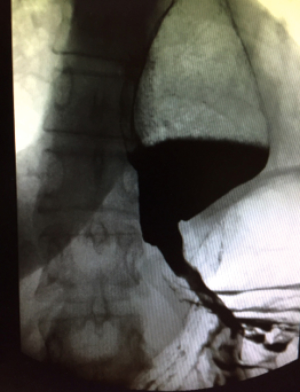
Patients are prepared for re-do POEM exactly as for primary intervention. A clear liquid diet for several days and pre-operative antibiotics are used. General endotracheal anesthesia with paralysis is employed. An initial diagnostic endoscopy is performed to confirm that the lower esophageal sphincter (LES) is indeed tight and that there are no other lesions present. Retained food or liquid in the esophagus is removed and if excessive, the case may need to be cancelled in order to more thoroughly empty the esophagus. A small clear plastic cap is affixed to the distal end of the endoscope. Once again, a point 10 to 15 centimeters proximal to the esophagus-gastric junction is chosen to begin the tunnel. In cases of type 3 achalasia a more proximal point may be chosen to provide a longer myotomy. The point of injection and planned tunnel should be in a site opposite that of the original intervention. In cases of previous Heller myotomy that usually means lateral or posterior (Figure 3). When the first procedure was a POEM, the new site again should be on the opposite wall. The site chosen after previous failed pneumatic dilation does not matter. The tunnel is created after a submucosal injection of saline and a mucosal incision. The tunnel must be continued distally for several centimeters onto the gastric wall. The latter may be assured by a number of means, but this author uses fluoroscopy with the scope in the distal tunnel to assure that the tip of the scope is well below the diaphragm and into the gastric bubble (Figure 4). Following completion of the tunnel, the scope is withdrawn to several centimeters from the proximal entry site and the myotomy is commenced. It is only necessary to divide the circular muscle layer but this must be complete. The myotomy extends to the most distal end of the tunnel. Hemostasis must assure. Prior to closing the tunnel, the endoscope should be advanced through the native esophagus into the stomach to ensure that the esophagogastric junction is completely lax. If it is still tight, additional myotomy maybe required. Finally, the initial mucosotomy is closed with clips or suture. A postoperative water soluble esophagram is usually obtained the following day to assure free passage of liquid into the stomach and assure the absence of a leak. Patients are usually discharged on the first postoperative day and maintained on a full liquid diet for one week.

Results
Several studies of re-operative POEM have demonstrated high success rates after previously failed POEM, Heller myotomy, and pneumatic dilation. In the long term however, progression of the underlying disease may cause the patients to present years later with recurrent dysphagia. In a number of these cases there persists poor esophageal emptying in spite of a widely patent gastroesophageal junction. This is often associated with megaesophagus, and when severe, esophagectomy may need to be considered (Figure 5).
Conclusions
POEM has emerged as a safe and effective therapeutic primary modality in the treatment of achalasia. When treatment failure occurs after Heller myotomy, pneumatic dilation, or POEM, repeat POEM is a good option to consider to improve the ultimate outcome.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (David W. Rattner, Ozanan Meireles) for the series “Update on the Diagnosis and Treatment of Achalasia” published in Journal of Xiangya Medicine. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2018.12.03). The series “Update on the Diagnosis and Treatment of Achalasia” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Inoue H, Minami H, Kobayashi Y, et al. Peroral endoscopic myotomy (POEM) for esophageal achalasia. Endoscopy 2010;42:265-71. [Crossref] [PubMed]
- Pasricha PJ, Hawari R, Ahmed I, et al. Submucosal endoscopic esophageal myotomy: a novel experimental approach for the treatment of achalasia. Endoscopy 2007;39:761-4. [Crossref] [PubMed]
- Bhayani NH, Kurian AA, Dunst CM, et al. A comparative study on comprehensive, objective outcomes of laparoscopic Heller myotomy with per-oral endoscopic myotomy (POEM) for achalasia. Ann Surg 2014;259:1098-103. [Crossref] [PubMed]
- Litle VR. Laparoscopic Heller myotomy for achalasia: a review of the controversies. Ann Thorac Surg 2008;85:S743-6. [Crossref] [PubMed]
- Vigneswaran Y, Yetasook AK, Zhao JC, et al. Peroral endoscopic myotomy (POEM): feasible as reoperation following Heller myotomy. J Gastrointest Surg 2014;18:1071-6. [Crossref] [PubMed]
Cite this article as: Ponsky JL. Per-oral endoscopic myotomy after previous interventions for achalasia. J Xiangya Med 2019;4:5.


