Propeller perforator flaps for finger reconstruction
Introduction
The reconstruction of finger defects can be sometimes challenging especially in the distal part. A lot of surgical procedures were and are still successfully used, i.e. free flaps from the foot, free venous flaps, V-Y advancement flaps, distally or proximally based neurovascular island flaps, cross-finger flaps, thenar or hypothenar flaps, but every one of them with advantages and disadvantages. A good coverage should provide a very similar material, which should offer a very good sensibility, stability and resistance. So, the use of flaps harvested from the closed vicinity seems to remain the most reasonable choice. To avoid at least some of the disadvantages of other methods, Koshima et al. described in 2006 the digital artery perforator flap (DAP) for fingertip reconstruction (1). We extended the use of this flap also for more proximal defects in the fingers and also for the thumb. To avoid the single disadvantage of this flap—the necessity of grafting, sometimes, the donor site—we imagined the use of the digital artery perforator flap as a bi-lobed digital artery perforator flap (BLDAP).
Anatomical considerations
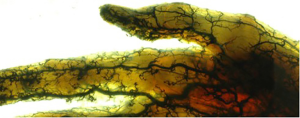
Our experimental work on fresh cadaver specimens (transparentation of cadaver degloved hand skin injected with latex) confirmed the findings of Koshima et al. (1). We found many small branches emerging from the proper digital arteries on both lateral and medial aspect of the fingers (Figure 1). These small vessels perforate the thin fascia and subcutaneous tissue to end through multiple arterioles into the subdermal layer and realize very rich anastomoses at the level of the lateral and medial midline of the fingers (1-3). Even that usually the proper digital arteries have no comitant veins (4), sometimes can be found double or single comitant veins (1). So, usually, small venules in the fatty layer connecting to the dorsal and palmar veins realize the venous drainage (1). Small branches of the digital nerves accompany also the vascular network (1). Kostopoulos et al. described the vascular cutaneo-tendino-osseous complex, which originates from the proper digital arteries and is responsible of the vascularization of skin, extensor apparatus and periosteum (4,5).
Flap harvesting
Even if some authors detect the perforators by using a Doppler device (1), knowing that the location of perforators originating from the proper digital arteries is constant in relation to the digital joints, their preoperative Doppler detection is not mandatory (5). The design and harvesting of such a microsurgical non-microvascular flap should respect the principle of a free-style local perforator flap (5,6).
Design of the flap
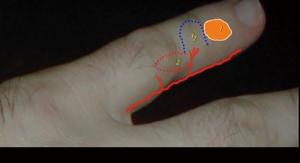
Depending to the location of the defect, the flap is designed with one of its edges corresponding to one of defect edges, either proximal or distal to it (Figure 2). The flap is preliminary designed intraoperative, on the lateral or medial aspect of the finger, by respecting the functional border of the respective finger (Figure 3). The final design of the flap will be done only after finding the perforator on which the flap will be based (see Figure 4). The length of the flap can be up to 4cm, and its width up to 1.5–2 cm. After finding the right perforator, it is very important to add few millimeters to the length of the flap, measured from the location of the perforator to the most proximal/distal edge of the flap, and also to its width, to avoid any tension (see Figure 4). It is not always necessary to visualize and squeletonize the perforator. Sometimes is enough to leave, at the level of the pivot point, only some subcutaneous tissue containing superficial arterioles able to vascularize the flap (1) (Figures 3,5).


Harvesting the flap
Step 1
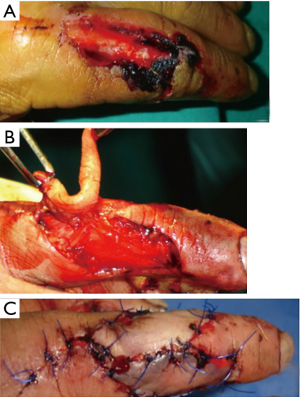
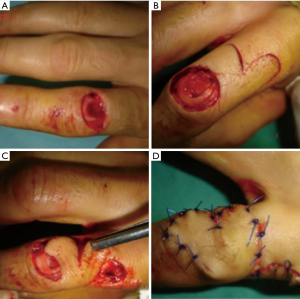
After measuring the defect, a preliminary design of the flap is completed (Figure 3).
Step 2
The dorsal or palmar edge of the flap is incised (Figure 3) and the undermining is performed in a subfascial plan, but by preserving the paratenon of the extensor apparatus (see Figure 6). After finding the right perforator as close as possible to the defect, the incision around the flap is completed. Even if the perforator is skeletonized, is better to leave a small cuff of subcutaneous tissue around it to avoid the possible spasm and to ensure the venous drainage of the flap. This will increase also the chances to obtain a faster re-innervation of the flap.
Step 3
The harvesting of the flap is then completed, by proceeding from proximal to distal, superficial to the proper neurovascular pedicle (Figures 3,6). The flap is then rotated for 90 to 180 degrees into the defect and sutured under no tension. Care should be taken to rotate the flap in the right way to avoid the twist or constriction of the pedicle (Figure 6).
Step 4
For the flaps with a width up to 1cm, the donor site can be directly closed after slight undermining of the edges of the donor site (Figure 3). In case of larger flaps, the donor site should be covered with split thickness skin graft (Figure 5).
To avoid this disadvantage, and knowing the existence of rich anastomoses at the level of the lateral and medial midline of the fingers, it is possible to use a pedicled bi-lobed flap, in which procedure the two lobes are used as transposition flaps rotated usually for at least 90 degrees each: the first lobe will cover the defect and is designed transversally or slightly oblique, and the second lobe, designed longitudinally, will cover the donor site of the first flap (Figure 7). If the first flap should be usually few millimeters longer and larger, the second flap should have a maximum width of 2/3 from the width of the first one. This will allow the direct closure of the second flap donor site (Figure 8).
Knowing the existence of the so called vascular cutaneo-tendino-osseous complex described by Kostopoulos et al. (4,5), it is evident that a complex defect affecting also the extensor apparatus can be reconstructed by using a composite flap including a small slip of vascularized tendon (Figures 8,9).

Discussion
A lot of methods were described in the attempt to preserve the length of the fingers or to cover exposed vital anatomical elements in the fingers. The skin over the palmar aspect of the fingers is a very specialized one, and so the necessity to reconstruct it by replacing like with like is more than evident.
The use of free flaps from the foot (10) or of free venous flaps (11) is reliable methods, but they require microsurgical techniques, which are not always available or possible to be performed by the beginners.
A good coverage should provide a very similar material, which should offer a very good sensibility, stability and resistance. So, the use of flaps harvested from the closed vicinity seems to remain the most reasonable choice. Various methods of reconstruction by using local resources were described, such as V-Y advancement flaps (12,13) (which, sometimes, are too small or cannot provide enough advancement), distally (14) or proximally (15) based neurovascular island flaps (with the disadvantage of extensive dissection of the pedicle, sectioning of the pedicle in the distal variant, and often the skin grafting of the donor site), cross-finger flaps (16), thenar (17) or hypothenar flaps (18) (which need second stage surgery).
The DAP flap, described by Koshima (1) avoids most of the disadvantages of these methods. First of all, it allows the reconstruction like-with-like of the supraspecialized palmar skin. Then, for a width of the flaps less than 1 cm, the donor site can be closed by direct suture, what avoids the possible retraction of a skin graft. But, even in some cases it is not possible to avoid the skin grafting, we avoid this disadvantage by using the BLDAP.
Both the DAP and BLDAP are very well blood supplied, either through a main perforator of the proper digital artery or through the small arterioles into the subcutaneous tissue (1). The venous drainage, either through the comitant vein(s), when exist, or through the small venules into the subcutaneous tissue (1). Even if there are only small series until now, the high rate of successful cases proves the robust anatomy and reliability of these flaps, with very good long-term results (Figures 9,10). No venous congestion or other complications were reported in the series of Xianyu et al. (7 cases of innervated DAP flaps) (19), Li et al. (3 cases of innervated DAP flaps) (20), Pelissier et al. (27 cases of DAP flaps) (21). In a series of 15 DAP flaps, Kostopoulos et al. had a 100% success rate, without any venous congestion, and with only one case presenting a minor wound dehiscence (5). A partial skin necrosis was reported in the series of Mitsunaga et al. (in 2 cases out of 13) (22) and of Basat et al. (in one case out of 5 cases) (23).

The main indications of the DAP and BLDAP flaps include the preservation of the length of amputation stumps, the replacement of stumps’ scaring skin, the coverage of post-excisional defects, the reconstruction of some complex defects involving skin and extensor apparatus.
Conclusions
The main advantages of DAP and BLDAP flaps, i.e., sparing the neurovascular pedicles, replacing like-with-like, faster reinnervation, less invasive and very short surgery, the possibility to directly close the donor site in most of the cases, recommend these flaps as a new and valuable alternative in digital reconstruction.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Geoffrey Hallock, Juyu Tang) for the series “Perforator Flap” published in Journal of Xiangya Medicine. The article has undergone external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2018.04.07). The series “Perforator Flap” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Koshima I, Urushibara K, Fukuda N, et al. Digital artery perforator flaps for fingertip reconstructions. Plast Reconstr Surg 2006;118:1579-84. [Crossref] [PubMed]
- Endo T, Kojima T, Hirase Y. Vascular anatomy of the finger dorsum and a new idea for coverage of the finger pulp defect that restores sensation. J Hand Surg Am 1992;17:927-32. [Crossref] [PubMed]
- Strauch B, de Moura W. Arterial system of the fingers. J Hand Surg Am 1990;15:148-54. [Crossref] [PubMed]
- Kostopoulos E, Casoli V, Verolino P, et al. Arterial blood supply of the extensor apparatus of the long fingers. Plast Reconstr Surg 2006;117:2310-8. [Crossref] [PubMed]
- Kostopoulos E, Agiannidis C, Konofaos P, et al. Predictable pattern digital artery perforator flap: an alternative concept in digital reconstruction. Hand 2016;11:88-96. [Crossref] [PubMed]
- Georgescu AV, Matei I, Ardelean F, et al. Microsurgical nonmicrovascular flaps in forearm and hand reconstruction. Microsurgery 2007;27:384-94. [Crossref] [PubMed]
- Georgescu AV, Matei IR. Tip amputation of the 5th finger: preliminary design, exploratory incision, and identification of a perforator on the medial aspect of the middle and distal phalanx; after knowing the exact location of the perforator, the final design of the flap is completed. Asvide 2018;5:499. Available online: http://www.asvide.com/article/view/24632
- Georgescu AV, Matei IR. Tip amputation of the 5th finger: the incision around the flap is completed, and the flap harvesting from proximal to distal is performed. Asvide 2018;5:500. Available online: http://www.asvide.com/article/view/24633
- Georgescu AV, Matei IR. Skin and extensor tendon defect on the PIP joint: long term postoperative result. Asvide 2018;5:501. Available online: http://www.asvide.com/article/view/24634
- Koshima I, Inagawa K, Urushibara K, et al. Fingertip reconstruction using partial-toe transfers. Plast Reconstr Surg 2000;105:1666-74. [Crossref] [PubMed]
- Kayikçioğlu A, Akyürek M, Safac T, et al. Arterialized venous dorsal digital island flap for fingertip reconstruction. Plast Reconstr Surg 1998;102:2368-72; discussion 2373. [Crossref] [PubMed]
- Kutler W. A method for repair of finger amputation. Ohio State Med J 1944;40:126.
- Atasoy E, Ioakimidis E, Kasdan ML, et al. Reconstruction of the amputated finger tip with a triangular volar flap. J Bone Joint Surg Am 1970;52:921-6. [Crossref] [PubMed]
- Niranjan NS, Armstrong JR. Homodigital reverse pedicle island flap in soft tissue reconstruction of the finger and the thumb. J Hand Surg Br 1994;19:135-41. [Crossref] [PubMed]
- O’Brien B. Neurovascular island pedicle flaps for terminal amputations and digital scars. Br J Plast Surg 1968;21:258-61. [Crossref] [PubMed]
- Tempest MN. Cross finger flaps in the treatment of injuries of the finger tip. Plast Reconstr Surg 1946;1952:205-22. [PubMed]
- Melone CP, Beasley RW, Carotens JH. The thenar flap: An analysis of its use in 150 cases. J Hand Surg Am 1982;7:291-7. [Crossref] [PubMed]
- Gu YD. Hypothenar flap. J Hand Surg 1997;2:149-53. [Crossref]
- Xianyu M, Lei C, Laijin L, et al. Reconstruction of finger-pulp defect with a homodigital laterodorsal fasciocutaneous flap distally based on the dorsal branch of the proper palmar digital artery. Injury 2009;40:1346-50. [Crossref] [PubMed]
- Li YF, Cui SS. Innervated reverse island flap based on the end dorsal branch of the digital artery: surgical technique. J Hand Surg Am 2005;30:1305-9. [Crossref] [PubMed]
- Pelissier P, Casoli V, Bakhach J, et al. Reverse dorsal digital and metacarpal flaps: a review of 27 cases. Plast Reconstr Surg 1999;103:159-65. [Crossref] [PubMed]
- Mitsunaga N, Mihara M, Koshima I, et al. Digital artery perforator (DAP) flaps: modifications for fingertip and finger stump reconstruction. J Plast Reconstr Aesthet Surg 2010;63:1312-7. [Crossref] [PubMed]
- Basat SO, Ugurlu AM, Aydin A, et al. Digital artery perforator flaps: an easy and reliable choice for fingertip amputation reconstruction. Acta Orthop Traumatol Turc 2013;47:250-4. [Crossref] [PubMed]
Cite this article as: Georgescu AV, Matei IR. Propeller perforator flaps for finger reconstruction. J Xiangya Med 2018;3:20.