
A pragmatic evaluation of the role of the medial sural artery perforator flap
Introduction
Although not considered by many to be a major or indispensable perforator flap, the medial sural artery perforator (MSAP) flap has some unique attributes that may make it a preferable choice in certain circumstances. Like all “true” perforator flaps (1), its perforasome allows capture of the same skin territory as would the medial gastrocnemius musculocutaneous flap; but leaves the muscle relatively intact to permit function preservation. Interestingly, even early in the history of free flaps this was considered a potential donor site as shown in cadaver dissections by Taylor and Daniel [1975] (2); but it was not until Cavadas et al. [2001] (3) before pragmatic clinical utilization was really initiated.
The MSAP flap has a potentially long vascular pedicle which allows formation of an island flap that can reach even to the patella or lower thigh (4). The pedicle itself can serve as the recipient site about the knee to avoid vein grafts or deeper dissection if a free flap in that region is needed (5). Even in the obese individual, the flap is relatively thin, providing an alternative to the comparably thin radial forearm flap (6). Others have shown an occasional role for challenges in the head & neck (7-9), hand (10), or upper extremity (11). The major drawback remains the donor site where any scar, since always quite conspicuous, would be unacceptable—especially for women. Consequently, some would suggest that maybe it’s only legitimate role without question would be for a lower extremity defect which is already aesthetically compromised (12).
Surgical anatomy
The medial sural artery and vein are branches of the respective popliteal vessels, arising at about the level of the knee joint. The artery at this point may have a 1–2 mm. inner diameter which is quite large (13). These vessels then pass a few centimeters before entering the hilum at the undersurface of the medial gastrocnemius muscle. Dusseldorp et al. (14) have described three intramuscular branching patterns, which really are pertinent only as a warning that these may course superficially or deep within the muscle, with the latter pattern making the intramuscular dissection of the requisite perforator even more difficult!
Although the exact number of usable musculocutaneous perforators of the medial gastrocnemius muscle is highly variable, at least one acceptable perforator will be found in every individual in this territory; although that could arise from a lateral sural artery or median sural artery perforator instead (14). The mean distance from the midpoint of the popliteal crease to that first perforator is 10 cm, and to the most distal perforator 16 cm.; but none are found less than 6 cm nor more than 18 cm away (13). Most will be found in the upper 1/5 or 1/3 of the lower leg where the belly of the medial gastrocnemius is readily visualized (13). Depending on the chosen perforator, the pedicle length will vary from 9–16 cm (13).
Flap design
A template to mark the boundaries of the desired flap should be centered over an acceptable MSAP, or eccentric distally to it if a longer pedicle length is desired. The problem is how to find that perforator. Pre-operative imaging studies really add little to using the ubiquitous handheld acoustic Doppler that is passed about a line drawn from the midpoint of the popliteal crease to the prominence of the medial malleolus, while staying within the upper 1/3 of the calf (Figure 1) (15), although thermography (see article in this series by Muntean et al. “Dynamic Infrared Mapping of Cutaneous Perforators.”) may change this approach. Once a perforator is discovered, the outline of the flap should be drawn with a longitudinal axis, as Saint Cyr has shown that perforasome interconnections in the lower extremity best assume such an orientation (16).

It must be understood that the actual flap boundaries usually will be altered once that perforator is specifically visualized at the time of surgical exploration; as unlike other perforator flaps, once the MSAP exits the muscle it takes a rambling subfascial course that allows stretch during ambulation before then piercing the deep fascia.
Flap harvest
The patient is placed flat on the surgical table if in a prone position, or with the hip abducted, lower leg externally rotated and knee flexed if supine. To enhance recognizing all structures including veins, a bloodless field is preferred by the exsanguination of the limb only by elevation before inflation of a mid-thigh tourniquet. A small 1–2 cm long incision is made parallel and about 2 cm below the posterior tibial border, just superior to where the desired perforator was found using the audible Doppler. This incision is extended through the deep fascia to expose the medial gastrocnemius muscle. With that pushed away from the deep fascia, a 5-mm 30° angled endoscope is introduced to verify the exact perforator location (17); or an exploratory incision via the upper flap boundary can just be made larger for direct perforator visualization. Once confirmed, the flap borders are redesigned if necessary.
Assuming a supine position, the medial border of the flap is next completely incised through the deep fascia to provide unimpeded exposure of the perforator, with the flap then dropped back by gravity onto a pile of towels that prevent stretch of that perforator while flap harvest is finished. The muscle is split above and below the perforator to expose its intramuscular course, followed by the necessary tedious intramuscular dissection until a large medial sural branch is encountered. That more readily is dissected back toward the popliteal crease until the desired pedicle length or caliber has been reached. The remaining flap boundaries can then be released to make this an island flap attached only by its vascular pedicle.
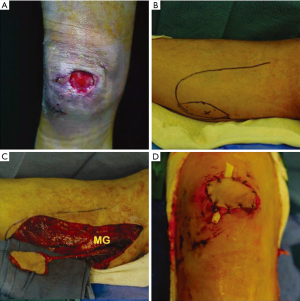
Once the pedicle dissection is finished, the tourniquet is deflated to check flap perfusion. Bleeding points are controlled. The flap is transferred where necessary as a local (Figure 2) or free flap (Figures 3,4). The donor site is closed using a running absorbable suture to repair any muscle rent. Primary skin closure is possible usually if the flap is less than 5 cm. in width, or otherwise a skin graft is necessary to prevent causing a compartment syndrome (18). If used as a local flap, great care must be observed to immobilize the limb without pressure on the vascular pedicle, while preventing pedicle stretching by joint movement.

Discussion
The MSAP flap will never be the ideal soft tissue flap unlike what many consider is the anterolateral thigh flap (19). Although not a mainstream choice, an awareness of its attributes is valuable for that unique case where it would be the ideal local flap for proximal-third lower leg problems instead of the medial gastrocnemius muscle, or as a relatively thin free flap for anywhere in the body (Table 1).
Table 1
| Items |
| Preserves medial gastrocnemius muscle function (1) |
| Local flap for knee or distal thigh coverage (4) |
| Island flap with long vascular pedicle (4) |
| Variable caliber of choice to avoid supermicrosurgery (13) |
| Relatively thin flap even in the obese (6) |
| Harvest possible in either the prone or supine position (6) |
| Chimeric flap possibilities when combined with muscle, tendon, medial sural nerve or lesser saphenous vein (20) |
| Spinal anesthesia alone satisfactory for lower limb reconstructions (13) |
| Sequential advancement or propeller flap to minimize the donor defect of the distal-based sural flap (21) |
MSAP, medial sural artery perforator.
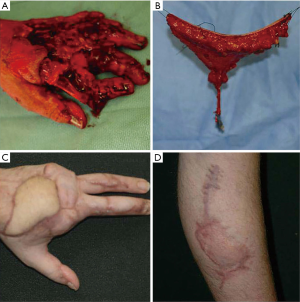
For many, the relatively thin MSAP flap has supplanted use of the radial forearm flap (9), thereby avoiding sacrifice of a major hand source vessel that for most hand surgeons would now be unacceptable (Figure 4). There are some justifiable concerns that must be recognized before selection of this flap is appropriate (Table 2). The greatest detriment will always remain the deformity created at the donor site. Even a linear scar will in general be too obvious (Figure 3), or even more so if skin grafted (Figure 4), that from an aesthetic standpoint, most patients would consider this an absolute contraindication for making this the flap of choice.
Conclusions
If the ultimate donor site appearance is of paramount importance, selection of the MSAP flap alternative should be avoided. However, as a local flap, this has replaced the traditional role of the medial gastrocnemius muscle, thereby preserving the latter’s function. As a free flap with a potentially long pedicle of large caliber, few could argue that use for ipsilateral lower limb defects would be a legitimate indication, as this would restrict all intervention to a single body region that has already been to some degree traumatized.
Acknowledgments
David C. Rice, B.S., Physician Extender, helped assist all cases.
Funding: None.
Footnote
Provenance and Peer Review: The article was commissioned by the editorial office, Journal of Xiangya Medicine for the series “Perforator Flap”. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2018.04.04). The series “Perforator Flap” was commissioned by the editorial office without any funding or sponsorship. GH served as the unpaid Guest Editor of the series and serves as an unpaid editorial board member of Journal of Xiangya Medicine from Apr 2017 to Mar 2019. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Wei FC, Jain V, Suominen S, et al. Confusion Among Perforator Flaps: What is a True Perforator Flap? Plast Reconstr Surg 2001;107:874-6. [Crossref] [PubMed]
- Taylor GI, Daniel RK. The Anatomy of Several Free Flap Donor Sites. Plast Reconstr Surg 1975;56:243-53. [Crossref] [PubMed]
- Cavadas PC, Sanz-Gimenez-Rico JR, Gutierrez-de la Camara A, et al. The Medial Sural Artery Perforator Free Flap. Plast Reconstr Surg 2001;108:1609-15. [Crossref] [PubMed]
- Kosutic D, Pejkovic B, Anderhuber F, et al. Complete Mapping of Lateral and Medial Sural Artery Perforators: Anatomical Study with Duplex-Doppler Ultrasound Correlation. J Plast Reconstr Aesthet Surg 2012;65:1530-6. [Crossref] [PubMed]
- Kim KN, Kim SI, Ha W, et al. Popliteal Fossa Reconstruction with a Medial Sural Artery Perforator Free Flap Using the Medial Sural Vessel as the Recipient. J Plast Surg Hand Surg 2017;51:387-92. [Crossref] [PubMed]
- Hallock GG, Sano K. The Medial Sural MEDIAL GASTROCNEMIUS Perforator Free Flap: an “Ideal” Prone Position Skin Flap. Ann Plast Surg 2004;52:184-7. [Crossref] [PubMed]
- Chen SL, Chen TM, Dai NT, et al. Medial Sural Artery Perforator Flap for Tongue and Floor of Mouth Reconstruction. Head Neck 2008;30:351-7. [Crossref] [PubMed]
- Shen H, Shen XQ, Lv Y, et al. Pharyngoesophageal Reconstruction With the Medial Sural Artery Perforator Flap After Total Laryngopharyngectomy: A New Method. Ann Plast Surg 2017;78:191-4. [Crossref] [PubMed]
- Kao HK, Chang KP, Wei FC, et al. Comparison of the Medial Sural Artery Perforator Flap with the Radial Forearm Flap for Head and Neck Reconstructions. Plast Reconstr Surg 2009;124:1125-32. [Crossref] [PubMed]
- Lin CH, Lin CH, Lin YT, et al. The Medial Sural Artery Perforator Flap: a Versatile Donor Site for Hand Reconstruction. J Trauma 2011;70:736-43. [Crossref] [PubMed]
- Ives M, Mathur B. Varied Uses of the Medial Sural Artery Perforator Flap. J Plast Reconstr Aesthet Surg 2015;68:853-8. [Crossref] [PubMed]
- Hallock GG. Medial Sural Artery Perforator Free Flap: Legitimate Use as a Solution for the Ipsilateral Distal Lower Extremity Defect. J Reconstr Microsurg 2014;30:187-92. [PubMed]
- Xie XT, Chai YM. Medial Sural Artery Perforator Flap. Ann Plast Surg 2012;68:105-10. [Crossref] [PubMed]
- Dusseldorp JR, Pham QJ, Ngo W, et al. Vascular Anatomy of the Medial Sural Artery Perforator Flap: a New Classification System of Intra-muscular Branching Patterns. J Plast Reconstr Aesthet Surg 2014;67:1267-75. [Crossref] [PubMed]
- Hallock GG. A primer of schematics to facilitate the design of the preferred muscle perforator flaps. Plast Reconstr Surg 2009;123:1107-15. [Crossref] [PubMed]
- Saint-Cyr M, Wong C, Schaverien M, et al. The Perforasome Theory: Vascular Anatomy and Clinical Implications. Plast Reconstr Surg 2009;124:1529-44. [Crossref] [PubMed]
- Shen XQ, Lv W, Shen H, et al. Endoscope-assisted Medial Sural Artery Perforator Flap for Head and Neck Reconstruction. J Plast Reconstr Aesthet Surg 2016;69:1059-65. [Crossref] [PubMed]
- Addison PD, Lannon D, Neligan PC. Compartment Syndrome After Closure of the Anterolateral Thigh Flap Donor Site: A Report of Two Cases. Ann Plast Surg 2008;60:635-8. [Crossref] [PubMed]
- Wei FC, Jain V, Celik N, et al. Have we found an ideal soft-tissue flap? An experience with 672 anterolateral thigh flaps. Plast Reconstr Surg 2002;109:2219-26. [Crossref] [PubMed]
- Han SE, Lee KT, Mun GH. Muscle-chimaeric Medial Sural Artery Perforator Flap: A New Design for Complex Three-dimensional Knee Defect. J Plast Reconstr Aesthet Surg 2014;67:571-4. [Crossref] [PubMed]
- Eser C, Gencel E, Kesiktaş E, et al. A convenient flap for repairing the donor area of a distally based sural flap: gastrocnemius perforator island flap. J Plast Reconstr Aesthet Surg 2016;69:1109-15. [Crossref] [PubMed]
Cite this article as: Hallock GG. A pragmatic evaluation of the role of the medial sural artery perforator flap. J Xiangya Med 2018;3:19.


