Laparoscopic complete mesocolic excision (CME) with completely medial approach for right-hemi colon cancer
Introduction
Surgical strategies of complete mesocolic excision (CME) includes two concepts based on embryonic anatomy and surgical oncology: sharp separation of the mesocolic visceral and parietal plane; radical lymph nodes dissection and ligation colon-feeding vessels at their roots for a larger range of longitudinal enterotomy (1). The feasibility and survival benefit of CME for the patients with colon cancer has been demonstrated recent years (2-5). Lateral and medial accesses are two modes of CME procedure. Conventional laparoscopic CME utilizes lateral access. Previous study has indicated that laparoscopic CME via medial access and traditional colectomy are technically comparative (4).
Completely medial approach (CMA) and hybrid medial approach (HMA) are two different approaches for medial access proposed by our medical center. CMA involves several bottom-to-top approaches including the entrance of intermesenteric space (IMS) via transverse retrocolic space (TRCS), the dissection of the middle colic vessels (MCV), the gastrocolic trunk of Henle (Henle trunk, HT) and the inferior margin of pancreas. Previous research has demonstrated that CMA is technically feasible, and is the better choice for right hemicolectomy (6). The main goal of this article is to illustrate the surgical procedures and anatomic strategies of CMA in details based on this case.
Method
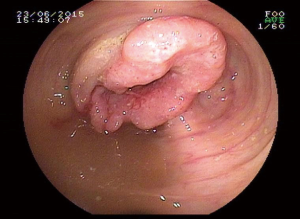
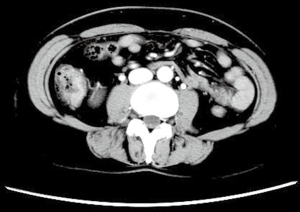
Patients with clinical stage II, III right-hemi colon cancer and whose important vessels in the surgical area are free from the invasion of tumor can be the candidate for CMA. Patients should have a well tolerability for laparoscopic surgery, and without severe cardiopulmonary insufficiency. In the present video (Figure 1), the patient is a 45 years old woman who was diagnosed adenocarcinoma of ascending colon proximal to hepatic flexure by coloscope and histological test (Figure 2). The tumor stage was assessed to be cT4N1M0 by CT scan preoperation (Figure 3).

Surgical position
The patient was placed in supine position after the administration of general anesthesia, with both legs split and arms folded, and at a head-down left side tilt position. The surgeon stood on the left side of the patient, while the first assistant was on the right. The camera operator was positioned between two legs of the patient.
Surgical procedures
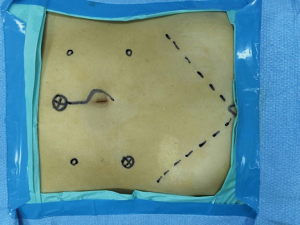
Pneumoperitoneum maintained not higher than 12 mmHg, and was built via the Veress needle. Five trocars were required in this surgery. One 10-mm trocar was placed on the upper left abdomen; the other was placed at the infraumbilical area with an inserted 30-degree laparoscope. One 5-mm trocar was on the lower left abdomen, and another two 5-mm trocars were on the upper and lower right abdomen respectively (Figure 4).
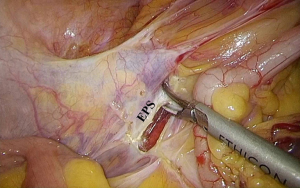
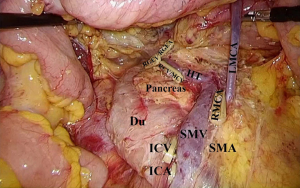
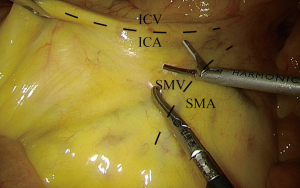
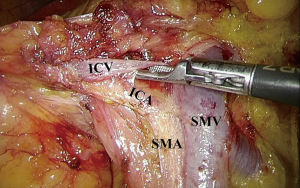
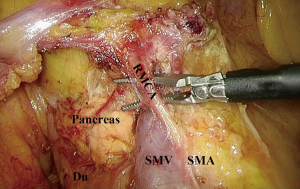
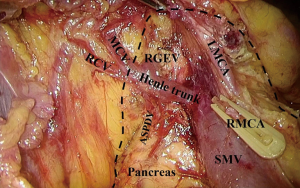
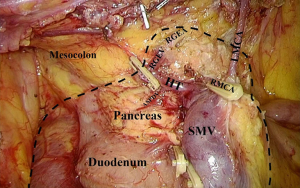
The surgical procedure of CMA starts at the ileocolic vessel and proceeds along superior mesenteric vein (SMV) to enter the TRCS from bottom to top. A bottom-to-top fashion is used to extend from pancreatic inferior edge. Middle colon vessels and the HT were dissected afterwards. TRCS is extended laterally to commute RRCS and superiorly to enter the IMS. Extending the inborn surgical plains to avoid mesocolon from defection. The surgery was conducted as follow (Figures 4,5,6,7,8,9,10,11,12,13).
Results
It took 128 min to finish this surgery, intraoperative bleeding was about 10 mL. Nineteen central lymph nodes were retrieved. The pathology outcome after the surgery shows it the adenocarcinoma staging T4N1M0. Besides, the time to first passing flatus and discharge were 2 and 12 days respectively.
Discussion
Anatomic strategies of CMA
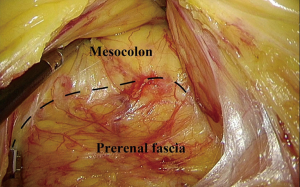
Laparoscopic CME via medial access completes the dissection of surgical trunk and the ligation of central vessel to mobilize colon, involving an approach of inferior medial to superior lateral. Three avascular spaces (TRCS, RRCS and IMS), and one surgical plane consists of gut, prerenal fascia (PRF) and nearby structure is essential to the mobilization of right-hemi colon (6).
IMS is located superior to the transverse mesocolon and posterior to the greater omentum. It communicates with the TRCS via the root of the transverse mesocolon. Thus, the entrance of the IMS is necessary for the mobilization of transverse mesocolon. CMA requires a bottom-to-top approach during the mobilization, which has the advantage of fewer vessel-related complications and reducing operation time.
Difficulties and obstacles in CMA to the CME
Recognize the TRCS
The TRCS is an inborn surgical space located posterior to the transverse mesocolon and anterior to the pancreatic inferior margin. We propose two ways to identify the TRCS. First, SMV can serve as a landmark for TRCS. In CMA, the range to dissect mesocolon can be clearly defined by the surface of SMV sheath, and the entrance of TRCS can be achieved after dissection. Second, TRCS can be successfully entered by superior extension of RRCS by dissecting the ventral part of the pancreas and the horizontal portion of duodenum.
“Climbing’’ the pancreatic inferior edge
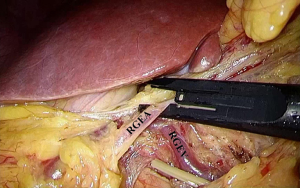
Hemorrhage of pancreatic injuries is a potential complication of CMA. Therefore, it’s vital to recognize the pancreatic inferior edge and the timing for ‘‘climbing’’. We regard emergence of the HT as the symbol of close to the pancreatic inferior edge. Meanwhile, the extension of the avascular space should be converted into a climbing procedure from bottom to top. Besides, it’s also feasible to dissect along the left margin of right gastroepiploic vein (RGEV) get entrance to IMS.
Conclusions
Laparoscopic CME for CMA is safe, technically feasible and highly recommended for the tumor locates in the right-hemi colon. Whereas, it’s also a difficult surgery that should be conducted in an experienced medical center.
Acknowledgments
The authors appreciate the contributions of their coworkers and friends to this study, as well as the editors and reviewers for their input.
Funding: The authors gratefully acknowledge the National High Technology Research and Development Program of China (863 Program), the Science and Technology Commission of Shanghai Municipality, and the Shenkang Center of Hospital Development for financial support (2012AA021103, 1141195070, 11411950701, SHDC12010116).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.04.08). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hohenberger W, Weber K, Matzel K, et al. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis 2009;11:354-64; discussion 364-5. [Crossref] [PubMed]
- Bertelsen CA, Neuenschwander AU, Jansen JE, et al. Disease-free survival after complete mesocolic excision compared with conventional colon cancer surgery: a retrospective, population-based study. Lancet Oncol 2015;16:161-8. [Crossref] [PubMed]
- Bokey L, Chapuis PH, Chan C, et al. Long-term results following an anatomically based surgical technique for resection of colon cancer: a comparison with results from complete mesocolic excision. Colorectal Dis 2016;18:676-83. [Crossref] [PubMed]
- Feng B, Sun J, Ling TL, et al. Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc 2012;26:3669-75. [Crossref] [PubMed]
- Zheng MH, Feng B, Lu AG, et al. Laparoscopic versus open right hemicolectomy with curative intent for colon carcinoma. World J Gastroenterol 2005;11:323-6. [Crossref] [PubMed]
- Feng B, Ling TL, Lu AG, et al. Completely medial versus hybrid medial approach for laparoscopic complete mesocolic excision in right hemicolon cancer. Surg Endosc 2014;28:477-83. [PubMed]
- Feng B, Ma J, Hong H, et al. Laparoscopic CME with CMA for right-hemi colon cancer. J Xiangya Med 2017. Asvide 2017;4:212. Available online: http://www.asvide.com/articles/1522
Cite this article as: Feng B, Yan X, Ma J, Hong H, Xue P, Zheng M. Laparoscopic complete mesocolic excision (CME) with completely medial approach for right-hemi colon cancer. J Xiangya Med 2017;2:47.