
Isolated left lung bronchiectasis: a rare presentation of H type tracheoesophageal fistula
Introduction
Tracheoesophageal fistula (TEF) constitute about 1 in 100,000 live births with H-type TEF is 4–5% of all, and has a variable clinical presentation and approach of surgical correction (1). The presentations are recurrent respiratory symptoms due to aspiration pneumonitis while feeding, cyanosis, and abdominal distension and usually diagnosed in late infancy or childhood (2). The common surgical approach is right cervicotomy, if the fistula is above the T2 vertebra and rarely thoracotomy required if fistula is below (3). We hereby report a case of H-type TEF presented to us at the age of 4 years with recurrent chest infection and isolated left side lung bronchiectasis require a thoracic approach for surgical correction as it was quite low. We present the following case in accordance with the CARE reporting checklist. Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Case presentation
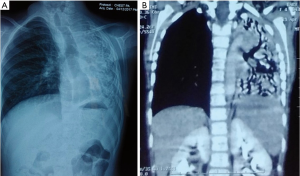
A 4-year-old female child presented with symptoms of recurrent pneumonitis since birth. There was a history of nasal and oral regurgitation of feeds, and required recurrent admission for pneumonia and left side bronchiectasis. The patient was referred to our hospital for the non-improvement of problem. On examination, respiratory rate was 45 per minute, decreased chest movements on the left side. On chest auscultation, there were decreased breath sounds on the left side. There were no other anomalies detected. Chest X-rays performed (Figure 1A) showed esophagus was grossly dilated, and air-filled, left side of chest show tram tracking appearance of dilated lower lobe bronchi suggestive of bronchiectasis. Esophagogram suggestive of H type fistula as contrast seen in the trachea. Contrast-Enhanced Computer Tomography (Figure 1B) was suggestive of bronchiectasis changes in the left lung field. Rigid bronchoscopy was performed under general anaesthesia and a diagnosis of H-type TEF was made at the level of T3 thoracic vertebra with purulent fluid was found in the left bronchus, aspirated and lavage done (Figure 2). TEF was repaired through the right thoracotomy extra pleural approach in the same setting of anaesthesia. The girl improved and was asymptomatic in the post-procedure duration. A follow-up of 8-month patient doing well with occasional cough. Radiography of thorax (including plain chest X-ray, contrast oesophagogram, and computer tomography of the thorax) demonstrates resolution of pulmonary bronchiectasis and there was a decrease in oesophageal diameter.
Discussion
The condition H type TEF, may present mild symptoms of repeated aspiration and pneumonia to life-threatening events. The symptoms may occur in the neonatal period to the oldest reported patient was 79 years old (4). The main symptoms of an H-TEF include recurrent pneumonitis, cyanosis, and choking on feeding and abdominal distension. Presentation like left lung isolated bronchiectasis in four years old girl child was not reported till date as found in our case. In our case, the fistula was quite low and towards left bronchus resulting in repeated aspiration and bronchiectasis. On plane chest X-ray, diagnosis is confirmed by an air-filled dilated esophagus due to constant inflation air from TEF in the esophagus (Figure 1A). In the case of an air-filled dilated esophagus, a possibility of TEF should always be considered. The mainstay of diagnosis is a water-soluble contrast oesophagogram which should be performed early in case of suspicious H-type fistula, and bronchoscopy should be done if the contrast esophagogram not show the fistula (5). There is a risk of aspiration pneumonia in contrast esophagogram. Rigid bronchoscopy is a better procedure to see the posterior wall of the trachea and can be gently probed to see the opening of a collapsed fistula. On rigid bronchoscopy, fistula can be cannulated with a guidewire, which aid identification of the fistula and repair. Rigid bronchoscopy helps determine the level of fistula, presence of unusual variants, e.g., double fistula, trifurcation fistula, presence and severity of tracheobronchitis, and position of the aortic arch (5). Most surgeons agreed that fistula at or above T2 should be approached through the cervical approach and fistula below this should be ligated by the thoracic approach (3,6-8). In our case, the fistula was at the T3 and we approached the fistula through the right thoracotomy. When the fistula was surgically divided our approach is to divide the TEF on the esophageal side to have sufficient amount tissue for good repair over posterior wall of the windpipe. The esophageal side has a tension-free closure due to the adequate width of the lumen and the interposition of vascularized tissue between repaired fistulas can prevent recurrence. Reported complications were fistula recurrence, esophageal stricture tracheomalacia, and left recurrent laryngeal nerve paralysis (9,10). Mortalities were usually rare if the condition is diagnosed and treated early.
Conclusions
The presentation of H type TEF may varied. Rigid bronchoscopy is diagnostic of H type TEF and surgical repair is curative of these anomalies.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at http://dx.doi.org/10.21037/jxym-20-57
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-20-57). The authors have no conflicts of interest to declare.
Ethical Statement:
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- de Jong EM, Felix JF, de Klein A, et al. Etiology of esophageal atresia and tracheoesophageal fistula: "mind the gap Curr Gastroenterol Rep 2010;12:215-22. [Crossref] [PubMed]
- Ng J, Antao B, Bartram J, et al. Diagnostic difficulties in the management of H-type tracheoesophageal fistula. Acta Radiol 2006;47:801-5. [Crossref] [PubMed]
- Parolini F, Morandi A, Macchini F, et al. Cervical/thoracotomic/thoracoscopic approaches for H-type congenital tracheo-esophageal fistula: a systematic review. Int J Pediatr Otorhinolaryngol 2014;78:985-9. [Crossref] [PubMed]
- Garand SA, Kareti LR, Dumont TM, et al. Thoracoscopic repair of tracheoesophageal fistula in a septuagenarian. Ann Thorac Surg 2006;81:1899-901. [Crossref] [PubMed]
- Jaiswala AA, Garg AK, Mohanty MK. ‘H’ type tracheo-oesophageal fistula – Case reports with review of the literature. Egyptian Journal of Ear, Nose Throat and Allied Sciences 2014;15:143-8.
- Genty E, Attal P, Nicollas R, et al. Congenital tracheoesophageal fistula without esophageal atresia. Int J Pediatr Otorhinolaryngol 1999;48:231-8. [Crossref] [PubMed]
- Mattei P. Double H-type tracheoesophageal fistulas identified and repaired in 1 operation. J Pediatr Surg 2012;47:e11-3. [Crossref] [PubMed]
- Karnak I, Senocak ME, Hiçsönmez A, et al. The diagnosis and treatment of H-type tracheoesophageal fistula. J Pediatr Surg 1997;32:1670-4. [Crossref] [PubMed]
- Crabbe DC, Kiely EM, Drake DP, et al. Management of the isolated congenital tracheo-oesophageal fistula. Eur J Pediatr Surg 1996;6:67-9. [Crossref] [PubMed]
- Genty E, Attal P, Nicollas R, et al. Congenital tracheoesophageal fistula without esophageal atresia. Int J Pediatr Otorhinolaryngol 1999;48:231-8. [Crossref] [PubMed]
Cite this article as: Rawat J, Singh G, Singh S. Isolated left lung bronchiectasis: a rare presentation of H type tracheoesophageal fistula. J Xiangya Med 2020;5:30.



