
Prolonged (continuous) prone position ventilation in a patient with a large mediastinal mass
Introduction
Maintenance of spontaneous ventilation and avoidance of general anesthesia are of paramount importance to prevent cardiorespiratory collapse in patients with large anterior mediastinal masses (1,2), When this is not possible, tracheal intubation and mechanical ventilation should be started. “Rescue therapy” for severe hypoxemic disease include Improve of mechanical ventilation with changes in body position, placement of a reinforced endotracheal tube distal to the obstruction, and cardiopulmonary By-pass (3-5).
Case report
Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Prone position in Acute Respiratory Distress syndrome (ARDS) is standard therapy for severe hypoxemic disease. Herein we report a case of a twenty-two years old woman with a large anterior mediastinal mass and pelerin edema who was admitted to the ICU with severe airway obstruction and bronchospasm after a percutaneous biopsy of the mediastinal mass and left thoracentesis. After tracheal intubation, pneumothorax was ruled out by chest x-ray and lung ultrasound; mechanical ventilation was optimized and high dose steroid therapy, salbutamol, ketamine and sevoflurane were prescribed; severe hypoxemia persisted (PaO2/FiO2 85), therefore she was ventilated in prone position (Figure 1).
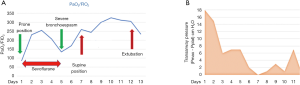
On day 5 after admission, pathology reported a diffuse type “B” large cell mediastinal lymphoma (Figure 2). Bone marrow was also infiltrated. After 12 days of mechanical ventilation, of which six of them were in prolonged continuous prone position (156 h), the patient was successfully extubated. The patient was discharged from the ICU to receive further chemotherapy.
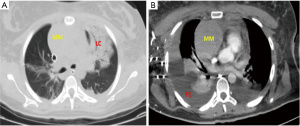
In this patient, the anterior mediastinal mass compressed vital structures as the heart and great vessels (pelerin edema) and produced tracheobronchial deviation/compression. These anatomical deviations and the resulted physiological alterations were barely “compensated” by the patient, and were lost after the diagnostic thoracentesis and percutaneous mediastinal mass biopsy were carried out. The catastrophic complications that followed included increased airway resistance and collapse (6), with concomitant severe hipoxemia and bronchospasm (increased transairway pressure).
Although more experience is needed (7-10), continuous prolonged prone position ventilation should be added as a rescue option in patients with airway obstruction and bronchospasm secondary to large anterior mediastinal masses.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym-20-31). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this study and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ferrari LR, Bedford RF. General anesthesia prior to treatment of anterior mediastinal masses in pediatric cancer patients. Anesthesiology 1990;72:991-5. [Crossref] [PubMed]
- Scheele B, Ascher K, De La Cuesta C, et al. Prone Positioning for Cardiorespiratory Collapse in an Adult Patient With Anterior Mediastinal Mass After General Anesthesia. Chest 2015;148:23A. [Crossref]
- Blank R, Souza D. Anesthetic management of patients with an anterior mediastinal mass: continuing professional development. Can J Anesth 2011;58:853-67. [Crossref] [PubMed]
- Castillo M, Slinger P. Myths of anterior mediastinal masses. South Afr J Anaesth Analg 2013;19:38-40. [Crossref]
- Datt V, Tempe DK. Airway management in patients with mediastinal masses. Indian J Anaesth 2005;49:344 52.
- Essandoh M. Anterior Mediastinal Mass Effects: It's Not Just About the Airway. J Cardiothorac Vasc Anesth 2020;34:1701. [Crossref] [PubMed]
- Hernández López GD, et al. Prone position ventilation in abdominal surgery patients complicated with acute respiratory distress syndrome: analysis of a cohort. Med Crit 2019;33:245-50.
- Hernández-López GD, Gorordo-Delsol LA, Jiménez-Ruiz A, Zamora-Gómez SE. Prone position ventilation for patients with severe ARDS and morbid obesity. Med Intensiva 2016;40:72. [PubMed]
- Dubey PK, Tripathi N. Anesthetic considerations in a patient with large anterior mediastinal mass. J Cardiothorac Vasc Anesth 2019;33:1073-5. [Crossref] [PubMed]
- Fabbro M, Patel PA, Ramakrishna H, et al. CASE 5-2014 challenging perioperative management of a massive anterior mediastinal mass in a symptomatic adult. J Cardiothorac Vasc Anesth 2014;28:819-25. [Crossref] [PubMed]
Cite this article as: Gasca-Aldama JC, Castañón González JA, Morales Morales AH. Prolonged (continuous) prone position ventilation in a patient with a large mediastinal mass. J Xiangya Med 2020;5:26.


