
Respiratory healthcare resource allocation in rural hospitals in Hunan, China: a cross-sectional survey
Introduction
Respiratory diseases are leading causes of death and disability worldwide. In the updated report on the top 10 common causes of death published by World Health Organization in 2017, 4 kinds of respiratory diseases were listed, including chronic obstructive pulmonary disease (COPD), lower respiratory tract infections, lung cancer and tuberculosis (1). Currently, respiratory diseases have become increasingly prevalent and caused a heavy financial burden in China, at least partly attributing to severe air pollution and uncontrolled tobacco use (2,3). According to the data from a recent national cross-sectional study, about 8.6% of the general Chinese adult population (equal to 99.9 million Chinese adults) had spirometry-define COPD. However, less than 10% of patients with COPD were aware of their condition and only 3% got accurate diagnosis by pulmonary function test (PFT) (4). Similarly, asthma was reported to affect 45.7 million Chinese adults but remained largely undiagnosed and undertreated (5). Therefore, it has been recognized that the prevention, control and cure of respiratory diseases and the promotion of respiratory health services is a top priority in the health sector.
Improvements in respiratory health services cannot be achieved without optimizing healthcare resource allocation. In 2015, Chinese State Council released the tiered medical scheme. This policy divides all hospitals in China into three tiers and encourages collaborations among different tiers within a region in order to provide better accessibility to health services for patients in rural areas (6). The tiered medical scheme defined a series of “common respiratory diseases in primary care setting”, including COPD, asthma, chronic pulmonary heart disease, adult community-acquired pneumonia, pulmonary tuberculosis, acute upper respiratory infections, acute tracheo-bronchitis and adult obstructive sleep apnea hypopnea syndrome. Chinese government emphasized that most patients with these diseases who are not in life-threatening conditions should be diagnosed and treated in local hospitals. Therefore, to achieve this goal, necessary respiratory health services for the diagnosis and treatment of these diseases, such as PFT, bronchoscopy, sleep monitoring, atomization therapy and mechanical ventilation, must be popularized not only in major hospitals in urban areas but also in local hospitals in rural areas.
China is the largest developing country and has the biggest population in the world. Rural residents account for about 45% of the whole population, and rural health service is the key component of the whole healthcare system. Even though rural healthcare system in China has been significantly improved since the enforcement of health reform in recent decades, there is still a large gap between rural and urban areas in terms of the access to and the quality of respiratory health services. The major cause of this problem is the lack of healthcare resources in rural areas, including necessary medical facilities and equipment, qualified healthcare professionals and basic medical techniques (5). For example, routine annual PFT is essential for proper diagnosis, treatment and long-term management for COPD and asthma. But without spirometers or clinical staffs who can correctly use spirometers and analyze the test report, PFT cannot be performed in local rural hospitals. In this case, many patients from rural areas choose to go to major hospitals in urban areas when acute exacerbation occurs, which subsequently causes much higher medical expenditure and increases the risk of more exacerbations. So far, poor access to comprehensive respiratory health services remains a serious problem to be solved in rural China.
Therefore, there is an urgent need to assess the respiratory healthcare resource allocation in rural China and analyze the present problems, as well as the reasons. In this study, we investigated the current respiratory healthcare resources, including their respiratory medicine specialty (RMS), basic facilities and equipment, clinical staffing and available medical techniques, in 48 rural hospitals in Hunan Province through a cross-sectional survey.
Methods
Study design and setting
In the present study, a cross-sectional survey was performed among 48 rural hospitals located in 13 cities and 44 counties in Hunan Province, China (all the hospitals involved are listed in the Supplementary file). Hunan Province is located in middle China, which consists of 13 municipal administrative areas and 1 autonomous prefecture. The total area of Hunan is 210,000 square kilometers and the total population is 69 million. In the year of 2018, Hunan’s gross domestic product per capita is ranked 16th among all the 31 provinces in mainland China, which represents the average level of the whole country.
Data collection and processing
We designed a survey questionnaire of respiratory healthcare resources in rural hospitals, which focused on the establishment and development of RMS, the availability of facilities and equipment, the access to medical techniques, clinical staffing and the prevalence of respiratory diseases. This survey questionnaire was approved, distributed and collected by the Medical Policy and Management Office of Health Commission in Hunan Province, China. Thus, data authenticity was guaranteed in this study. Finally, data were extracted and analyzed by two analysts.
Content of questionnaire
The survey questionnaire included 5 aspects of inquiry content which were listed as follows: (I) the establishment of RMS, including the setup of the independent department of respiratory medicine, specialized outpatient service and intensive care unit (ICU), the department which provides smoking cessation service, and the bed number for hospitalized patients with respiratory diseases; (II) the availability of medical facilities and equipment including PFT laboratories, bronchoscopy rooms, sleep laboratories, atomization therapeutic rooms, non-invasive and invasive ventilators; (III) total number of clinical staffs (including specialist physicians and nurses in respiratory medicine) and their clinical training experiences; (IV) the application of medical techniques including mechanical ventilation, diagnostic bronchoscopy, therapeutic bronchoscopy, percutaneous lung biopsy and transbronchial needle aspiration (TBNA); (V) total number of patients who were diagnosed with respiratory diseases in these rural hospitals in the year of 2018. In this questionnaire, we mainly focused on the medical facilities, equipment and techniques that are necessary for the diagnosis and treatment of common respiratory diseases according to the tiered medical scheme promoted by Chinese government.
Statistical analysis
The Chi-square statistic was used to assess the differences of respiratory healthcare resource allocation between rural hospitals which had established an independent department of respiratory medicine and those hospitals which had not. A P value <0.05 was considered to be statistically significant. The software package SPSS Statistics Version 19.0 (IBM Corp., Armonk, New York, USA) was used for all of the analyses.
Results
The prevalence of respiratory diseases in rural hospitals
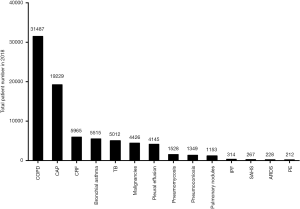
Total patient numbers for each kind of respiratory diseases in 48 rural hospitals were summarized in Figure 1. In the year of 2018, the top 5 common respiratory diseases included COPD (N=31,487), community-acquired pneumonia (N=19,229), chronic respiratory failure (N=5,965), asthma (N=5,515) and pulmonary tuberculosis (N=5,012). According to the tiered medical scheme, most patients of these diseases in rural areas are encouraged to be treated and managed in local hospitals instead of major hospitals in urban areas. These data indicated the heavy burden of respiratory health service for rural hospitals.
Department setup of RMS in rural hospitals
Even though rural hospitals are responsible for providing respiratory health services to a large population, the development of RMS in rural hospitals is limited and inequal due to the lack of financial support. As shown in Table 1, among 48 rural hospitals in Hunan, 58.3% (28/48) of them established an independent department of respiratory medicine, while other hospitals had a department of general internal medicine. Only half of these hospitals could provide respiratory specialized outpatient services; 12.5% (6/48) of them established an independent respiratory intensive care unit (RICU), and another 12.5% had comprehensive ICU; 47.9% (23/48) of these hospitals set up a department of smoking cessation. The average bed number for respiratory health services in each rural hospital was 58.
Table 1
| Department setup | Rural hospitals, N=48 (%) |
|---|---|
| Independent department of respiratory medicine | |
| Yes | 28 (58.3) |
| No | 20 (41.7) |
| Specialized outpatient service | |
| Yes | 24 (50.0) |
| No | 24 (50.0) |
| Intensive care unit | |
| Independent RICU | 6 (12.5) |
| Comprehensive intensive care unit | 6 (12.5) |
| No | 36 (75.0) |
| Smoking cessation service | |
| Yes | 23 (47.9) |
| No | 25 (52.1) |
| Average bed number for respiratory healthcare | 58 |
RICU, respiratory intensive care unit.
Available respiratory healthcare facilities and equipment in rural hospitals
As shown in Tables 2 and 3, 35 out of 48 rural hospitals had PFT laboratories and were equipped with 37 spirometers in total. Twenty-six out of 48 hospitals had bronchoscopy rooms and were equipped with 29 bronchoscopes; 64.6% (31/48) of these rural hospitals had 109 non-invasive ventilators, while 43.8% (21/48) had 29 invasive ventilators. Sleep laboratories were set up in only 6 hospitals and atomization rooms in 7 hospitals. Among 48 rural hospitals, only 2 hospitals had all of these basic medical facilities and equipment, indicating that a comprehensive scope of respiratory health services was not available in most rural hospitals.
Table 2
| Facilities and equipment | Total rural hospitals, N=48 (%) | Hospitals with independent RMS, N=28 (%) | Hospitals without independent RMS, N=20 (%) | P value |
|---|---|---|---|---|
| PFT laboratory | ||||
| Yes | 35 (72.9) | 23 (82.1) | 12 (60.0) | |
| No | 13 (27.1) | 5 (17.9) | 8 (40.0) | 0.089 |
| Bronchoscopy room | ||||
| Yes | 26 (54.2) | 20 (71.4) | 6 (30.0) | |
| No | 22 (45.8) | 8 (28.6) | 14 (70.0) | 0.005* |
| Sleep laboratory | ||||
| Yes | 6 (12.5) | 6 (21.4) | 0 (0.0) | |
| No | 42 (87.5) | 22 (78.6) | 20 (100.0) | 0.027* |
| Atomization room | ||||
| Yes | 7 (14.6) | 6 (21.4) | 1 (5.0) | |
| No | 41 (85.4) | 22 (78.6) | 19 (95.0) | 0.112 |
| Non-invasive ventilator | ||||
| Yes | 31 (64.6) | 20 (71.4) | 11 (55.0) | |
| No | 17 (35.4) | 8 (28.6) | 9 (45.0) | 0.241 |
| Invasive ventilator | ||||
| Yes | 21 (43.8) | 17 (60.7) | 10 (50.0) | |
| No | 27 (56.3) | 11 (39.3) | 10 (50.0) | 0.461 |
*, P<0.05 indicates statistical significance between rural hospitals with independent RMS and those without. RMS, respiratory medicine specialty; PFT, pulmonary function test.
Table 3
| Equipment category | Number of devices (%) | ||
|---|---|---|---|
| Total rural hospitals, N=48 | Hospitals with independent RMS, N=28 | Hospitals without independent RMS, N=20 | |
| Spirometer | 37 | 25 (67.6) | 12 (32.4) |
| Bronchoscope | 29 | 22 (75.9) | 7 (24.1) |
| Sleep monitor | 6 | 6 (100.0) | 0 (0.0) |
| Nebulizer | 42 | 34 (81.0) | 8 (19.0) |
| Non-invasive ventilator | 109 | 74 (67.9) | 35 (32.1) |
| Invasive ventilator | 29 | 15 (51.7) | 14 (48.3) |
RMS, respiratory medicine specialty.
To further assess the disparity of respiratory healthcare resources among rural hospitals, we compared the differences in medical facilities and equipment between hospitals with an independent RMS and those without. Our data showed that rural hospitals which established an independent department of respiratory medicine had better facilities and equipment than those without an independent department, and statistically significant differences could be seen between two groups in terms of bronchoscopy room (P=0.005) and sleep laboratory (P=0.027).
Respiratory healthcare staffs in rural hospitals
Table 4 presents the composition of respiratory healthcare staffs in rural hospitals. Totally there were 251 respiratory specialist physicians and 205 specialist nurses in 48 rural hospitals. The overall physician-to-bed ratio (PBR) was 1:11.1, and the nurse-to-bed ratio (NBR) was 1:13.6. In rural hospitals with an independent department of respiratory medicine, PBR was 1:10.3 and NBR was 1:11.9. While in rural hospitals without an independent department of respiratory medicine, PBR was 1:12.5 and NBR was 1:17.0. The proportion of respiratory physicians and nurses who received professional clinical training was also low in rural hospitals. Only 56.3% of rural hospitals had physicians who finished clinical training in intensive care units of grade IIIA hospitals (the first-class hospitals in urban areas of China), 54.2% had physicians who finished specialized ventilator training, 37.5% had physicians who finished respiratory therapy training, and 29.2% had physicians who finished PFT training. Besides, only 35.4% of rural hospitals had nurses who received ventilator training or respiratory therapy training. Not surprisingly, rural hospitals without independent RMS showed lower proportion of clinical staffs with professional clinical training. Significant differences were observed between two groups in physicians with ventilator training (P=0.024) and PFT training (P=0.014). These data revealed the shortage of clinical staffs, especially the shortage of physicians and nurses with subspecialty training experience, in rural hospitals.
Table 4
| Clinical staff composition | Total rural hospitals, N=48 (%) | Hospitals with independent RMS, N=28 (%) | Hospitals without independent RMS, N=20 (%) | P value |
|---|---|---|---|---|
| Number of physicians | 251 | 193 | 58 | – |
| Number of nurses | 205 | 184 | 21 | – |
| Physician-to-bed ratio | 1:11.1 | 1:10.3 | 1:12.5 | – |
| Nurse-to-bed ratio | 1:13.6 | 1:11.9 | 1:17.0 | – |
| Specialist physicians | ||||
| Yes | 46 (95.8) | 28 (100.0) | 18 (90.0) | |
| No | 2 (4.2) | 0 (0.0) | 2 (10.0) | 0.087 |
| Physicians | ||||
| With ICU training | 27 (56.3) | 18 (64.3) | 9 (45.0) | 0.184 |
| With ventilator training | 26 (54.2) | 19 (67.9) | 7 (35.0) | 0.024* |
| With RT training | 18 (37.5) | 13 (46.4) | 5 (25.0) | 0.131 |
| With PFT training | 14 (29.2) | 12 (42.9) | 2 (10.0) | 0.014* |
| Specialist nurses | ||||
| Yes | 34 (70.8) | 23 (82.1) | 11 (55.0) | |
| No | 14 (29.2) | 5 (17.9) | 9 (45.0) | 0.041* |
| Nurses | ||||
| With ventilator training | 17 (35.4) | 12 (42.9) | 5 (25.0) | 0.202 |
| With RT training | 17 (35.4) | 13 (46.4) | 4 (20.0) | 0.059 |
*, P<0.05 indicates statistical significance between rural hospitals with independent RMS and those without. RMS, respiratory medicine specialty; ICU, intensive care unit; RT, respiratory therapy; PFT, pulmonary function test.
Applicable respiratory medical techniques in rural hospitals
Respiratory medical techniques in 48 rural hospitals were summarized in Table 5. Mechanical ventilation was applicable in 32 rural hospitals. Diagnostic bronchoscopy was applicable in 47.9% of rural hospitals, while therapeutic bronchoscopy was applicable in only 6.3% of rural hospitals. Percutaneous lung biopsy and TBNA were applicable in 20.8% and 8.3% of rural hospitals, respectively. Rural hospitals with an independent department of respiratory medicine had statistically significant advantages over those without in the access to mechanical ventilation (P=0.038) and diagnostic bronchoscopy (P=0.001). Furthermore, based on the geographical locations of rural hospitals, we analyzed the availability of respiratory medical techniques in different municipal administrative areas in Hunan Province. Mechanical ventilation was available in all areas. Diagnostic bronchoscopy, TBNA, therapeutic bronchoscopy and percutaneous lung biopsy were retrospectively applicable in 92.3%, 30.8%, 15.4% and 46.2% of 13 municipal administrative areas (Table 6).
Table 5
| Medical techniques | Total rural hospitals, N=48 (%) | Hospitals with independent RMS, N=28 (%) | Hospitals without independent RMS, N=20 (%) | P value |
|---|---|---|---|---|
| Mechanical ventilation | ||||
| Yes | 32 (66.7) | 22 (78.6) | 10 (50.0) | |
| No | 16 (33.3) | 6 (21.4) | 10 (50.0) | 0.038* |
| Diagnostic bronchoscopy | ||||
| Yes | 23 (47.9) | 19 (67.9) | 4 (20.0) | |
| No | 25 (52.1) | 9 (32.1) | 16 (80.0) | 0.001* |
| TBNA | ||||
| Yes | 4 (8.3) | 4 (14.3) | 0 (0.0) | |
| No | 44 (91.7) | 24 (85.7) | 20 (100.0) | 0.077 |
| Therapeutic bronchoscopy | ||||
| Yes | 3 (6.3) | 3 (10.7) | 0 (0.0) | |
| No | 45 (93.8) | 25 (89.3) | 20 (100.0) | 0.131 |
| Percutaneous lung biopsy | ||||
| Yes | 10 (20.8) | 8 (28.6) | 2 (10.0) | |
| No | 38 (79.2) | 20 (71.4) | 18 (90.0) | 0.118 |
*, P<0.05 indicates statistical significance between rural hospitals with independent RMS and those without. RMS, respiratory medicine specialty; TBNA, transbronchial needle aspiration.
Table 6
| Medical techniques | Municipal administrative areas N=13 (%) |
|---|---|
| Mechanical ventilation | |
| Yes | 13 (100.0) |
| No | 0 (0.0) |
| Diagnostic bronchoscopy | |
| Yes | 12 (92.3) |
| No | 1 (7.7) |
| TBNA | |
| Yes | 4 (30.8) |
| No | 9 (69.2) |
| Therapeutic bronchoscopy | |
| Yes | 2 (15.4) |
| No | 11 (84.6) |
| Percutaneous lung biopsy | |
| Yes | 6 (46.2) |
| No | 7 (53.8) |
RMS, respiratory medicine specialty; TBNA, transbronchial needle aspiration.
As shown in Table 7, in the year of 2018, mechanical ventilation, diagnostic bronchoscopy, TBNA, therapeutic bronchoscopy and percutaneous lung biopsy were applied in 6,823, 6,001, 179, 68 and 457 patients in rural hospitals, respectively. More than 90% of these cases were performed in rural hospitals with independent RMS.
Table 7
| Medical techniques | Number of cases (%) | ||
|---|---|---|---|
| Total rural hospitals, N=48 | Hospitals with independent RMS, N=28 | Hospitals without independent RMS, N=20 | |
| Mechanical ventilation | 6,823 | 6,239 (91.4) | 584 (8.6) |
| Diagnostic bronchoscopy | 6,001 | 5,745 (95.7) | 256 (4.3) |
| TBNA | 179 | 179 (100.0) | 0 (0.0) |
| Therapeutic bronchoscopy | 68 | 68 (100.0) | 8 (0.0) |
| Percutaneous lung biopsy | 457 | 441 (96.5) | 16 (3.5) |
RMS, respiratory medicine specialty; TBNA, transbronchial needle aspiration.
Discussion
China has a population of more than 1.4 billion, and rural residents take up more than 40% of the whole population based on the statistics in 2016 (7). Rural hospitals are critical components of health system across the whole country due to their significant contributions to overall community well-being. In the present study, we found that, while rural hospitals were bearing a heavy burden of respiratory health services, the availability of healthcare resources were significantly underdeveloped in terms of basic facilities and equipment, clinical staffing and medical techniques. This imbalance is extremely serious in those rural hospitals which have not established an independent RMS.
Since the enforcement of health reform in 2009, Chinese government has achieved great accomplishments, including the expansion of social health insurance, the reform of public hospitals, and the strengthening of primary care (8). However, respiratory healthcare in rural areas of China are still facing challenges. Healthcare resource allocation imbalance is the key problem. Unlike America and Europe, hospitals in China are organized according to government administration and strictly hierarchized based on their scales, available armamentarium and techniques (7). Generally, rural hospitals, which are usually small-scale, have less facilities and equipment, and a small number of healthcare professionals, could not meet the basic needs of all local people. But meanwhile, more financial support from the government is flowing to major hospitals in urban areas instead of rural ones. Therefore, urban-to-rural disparity of resource allocation has been increasing, resulting in a vicious circle. Most rural residents do not have easy access to comprehensive and high-quality respiratory health services. Many patients may substitute local primary care providers for specialists or they may decide to postpone or forego healthcare from a respiratory specialist due to the heavy financial burdens and long travel time, which at least partially contributes to the low patient satisfaction in rural hospitals (9).
In this study, 48 rural hospitals provided respiratory health services across the continuum of care from primary care to long-term care for a total population of about 40 million in Hunan Province. Our data showed that 42.7% of these hospitals did not establish an independent department of respiratory medicine due to the lack of financial support and medical resources. Under such a condition, meeting the needs of patients for specialty care is difficult. Physicians and nurses in these hospitals must deal with a wide variety of general diseases every day, instead of concentrating on respiratory diseases. While they get comprehensive knowledge and skills of general internal medicine, they lose the opportunity to be trained as an outstanding respiratory specialist, which is obviously not good to provide high-quality subspecialty health services. Moreover, a considerable proportion of rural hospitals do not have basic facilities and equipment, including PFT laboratories, atomization room, bronchoscopes and ventilators. Total number of available devices for respiratory healthcare equipment is also small, especially in those hospitals without independent RMS. All these data reveal that respiratory diseases commonly seen in rural populations, such as COPD, asthma and pulmonary infection, are difficult to be accurately diagnosed and properly treated until they go to major hospitals in urban areas, which is contrary to the main principle of the national tiered medical scheme. Less than 15% of rural hospitals have set up sleep laboratories, indicating that sleep disorder is a weak point of respiratory health system in rural areas. Furthermore, application of respiratory medical techniques is also limited in rural hospitals based on our survey. Necessary diagnostic tools, including percutaneous lung biopsy and TBNA are not applicable in more than 79% of rural hospitals. Without a comprehensive diagnostic system for common respiratory diseases in primary care setting, it is extremely difficult to promote the quality of health services and patient satisfaction.
Based on our data, the overall PBR in rural hospitals is 1:11.1, and the overall NBR is 1:13.6, which is significantly lower when compared with most hospitals in urban areas of China and other developed countries (10-12). Heavy workload directly causes fatigue, which is associated with increased medical errors (13,14). It has been reported that up to 98,000 patients die each year in hospitals as a result of preventable medical errors, in which excess clinical workload is a main cause (15). Consistently, a higher PBR or NBR is associated with a better clinical outcome in patients with pneumonia and malignancies (10,12,16). On the other hand, the fact that a very low proportion of respiratory healthcare staffs in rural hospitals have received basic clinical training is also worrying. Most physicians and nurses have not undertaken any professional training on PFT, ventilator setup, respiratory therapy or respiratory intensive care. As a result, related clinical procedures may not be correctly performed, which could prolong hospital stays and even increase mortality of patients. It has been reported that an internship in a PFT laboratory significantly improved the technical and diagnostic skills of respiratory trainees (17). Thus, in order to improve the necessary knowledge and basic skills of rural healthcare professionals, more opportunities must be provided to those who are willing to participate clinical training on the diagnosis and treatment of common respiratory diseases. So there is an urgent need to attract more respiratory healthcare professionals, especially well-trained specialist physicians and nurses, to work in rural hospitals. The key is to improve the incomes and welfare of rural healthcare workers. The government must provide more financial support for rural hospitals to hire more qualified physicians and nurses, instead of keeping increasing the workload of the current clinical staffs.
A lack of specialist physicians has been a long-term problem in rural hospitals. Cultivation of more specialists is important to reduce the urban-to-rural disparity in high-quality health services. In a response to the nation’s call to integrate healthcare resources, with the joint effort of a group of leading Chinese and American pulmonary specialists, the formal subspecialty training program in the combined fields of pulmonary and critical care medicine (PCCM) throughout China was designed in 2014 (18). Subsequently, the Chinese Thoracic Society proposed collaborating with the American College of Chest Physicians to establish PCCM fellowship training program in China (19). So far, the Chinese Thoracic Society keeps enhancing and expanding PCCM training in urban and rural China, hopefully which will contribute to providing more specialists for rural hospitals. However, it is still too far to conclude on the beneficial effects of PCCM training program on rural hospitals due to the following issues. Firstly, the engagement of respiratory physicians from rural hospitals needs to be promoted. Till now, more than 300 fellows have enrolled and been trained with common curricula, educational activities, and assessment measures. But the proportion of trainees from rural hospitals is less than 10% overall. Furthermore, almost all the PCCM fellows from rural hospitals chose to work in higher-level hospitals after finishing the training program, which could lead to a brain drain in rural hospitals instead. Additionally, the final assessment examination for Chinese PCCM training fellows has been held in English so far, which is a big challenge for physicians from rural hospitals and directly reduce their enthusiasm to participate in this program. Thus, the Chinese Thoracic Society need to adjust this training program to Chinese healthcare system instead of completely copying the American pattern.
Conclusions
In summary, our data provides a view of current situation of respiratory healthcare resource allocation in rural China. Respiratory healthcare system in rural areas of China are facing great challenges, including a serious shortage of basic facilities and equipment, necessary medical techniques and qualified healthcare professionals. The results of this study may motivate policymakers to adopt suitable approaches to improve the respiratory healthcare resources in rural areas.
Supplementary
The list of rural hospitals involved in this study
People’s Hospital of Lianyuan City, Hunan, China
People’s Hospital of Jishou City, Hunan, China
People’s Hospital of Wugang City, Hunan, China
People’s Hospital of Hongjiang City, Hunan, China
People’s Hospital of Jiangyong County, Hunan, China
People’s Hospital of Fenghuang County, Hunan, China
People’s Hospital of Shuangfeng County, Hunan, China
People’s Hospital of Shuangpai County, Hunan, China
People’s Hospital of Guzhang County, Hunan, China
People’s Hospital of Longhui County, Hunan, China
People’s Hospital of Chengbu County, Hunan, China
People’s Hospital of Ningyuan County, Hunan, China
People’s Hospital of Anren County, Hunan, China
People’s Hospital of Anhua County, Hunan, China
People’s Hospital of Yizhang County, Hunan, China
People’s Hospital of Pingjiang County, Hunan, China
People’s Hospital of Cili County, Hunan, China
People’s Hospital of Xinhua County, Hunan, China
People’s Hospital of Xintian County, Hunan, China
People’s Hospital of Yongshun County, Hunan, China
People’s Hospital of Rucheng County, Hunan, China
People’s Hospital of Jianghua County, Hunan, China
People’s Hospital of Yuanling County, Hunan, China
People’s Hospital of Luxi County, Hunan, China
People’s Hospital of Zhongfang County, Hunan, China
People’s Hospital of Guidong County, Hunan, China
People’s Hospital of Yanling County, Hunan, China
People’s Hospital of Suining County, Hunan, China
People’s Hospital of Huitong County, Hunan, China
People’s Hospital of Xinhuang County, Hunan, China
People’s Hospital of Dongkou County, Hunan, China
People’s Hospital of Tongdao County, Hunan, China
People’s Hospital of Longshan County, Hunan, China
People’s Hospital of Xinning County, Hunan, China
People’s Hospital of Sangzhi County, Hunan, China
People’s Hospital of Shaoyang County, Hunan, China
People’s Hospital of Xinshao County, Hunan, China
People’s Hospital of Huayuan County, Hunan, China
People’s Hospital of Baojing County, Hunan, China
People’s Hospital of Xupu County, Hunan, China
People’s Hospital of Shimen County, Hunan, China
People’s Hospital of Qidong County, Hunan, China
People’s Hospital of Zhijiang County, Hunan, China
People’s Hospital of Chaling County, Hunan, China
People’s Hospital of Chenxi County, Hunan, China
People’s Hospital of Jingzhou County, Hunan, China
People’s Hospital of Mayang County, Hunan, China
The Second People’s Hospital of Anhua County, Hunan, China
Supplementary
Acknowledgments
The authors are grateful to all participants at the 48 rural hospitals where data collection occurred for their coordination and support throughout the study.
Funding: This study was funded by the National Natural Science Foundation of China (81873406) and the National Key Research and Development Program of China (2018YFC1311900).
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2020.02.05). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was reviewed and approved by the Ethical Committee of Central South University Xiangya Hospital (No. 2019030466). Informed consent was obtained from all participants for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Forum of International Respiratory Societies. The Global Impact of Respiratory Disease - Second Edition. Sheffield, European Respiratory Society 2017.
- Zhu B, Wang Y, Ming J, et al. Disease burden of COPD in China: a systematic review. Int J Chron Obstruct Pulmon Dis 2018;13:1353-64. [Crossref] [PubMed]
- Kan H. Environment and health in china: challenges and opportunities. Environ Health Perspect 2009;117:A530-1. [Crossref] [PubMed]
- Wang C, Xu J, Yang L, et al. Prevalence and risk factors of chronic obstructive pulmonary disease in China (the China Pulmonary Health [CPH] study): a national cross-sectional study. Lancet 2018;391:1706-17. [Crossref] [PubMed]
- Huang K, Yang T, Xu J, et al. Prevalence, risk factors, and management of asthma in China: a national cross-sectional study. Lancet 2019;394:407-18. [Crossref] [PubMed]
- Feng D, Zhang D, Li B, et al. Does having a usual primary care provider reduce patient self-referrals in rural China's rural multi-tiered medical system? A retrospective study in Qianjiang District, China. BMC Health Serv Res 2017;17:778. [Crossref] [PubMed]
- Sun Y, Gregersen H, Yuan W. Chinese health care system and clinical epidemiology. Clin Epidemiol 2017;9:167-78. [Crossref] [PubMed]
- Li L, Fu H. China's health care system reform: Progress and prospects. Int J Health Plann Manage 2017;32:240-53. [Crossref] [PubMed]
- Li J, Wang P, Kong X, et al. Patient satisfaction between primary care providers and hospitals: a cross-sectional survey in Jilin province, China. Int J Qual Health Care 2016;28:346-54. [Crossref] [PubMed]
- Yasunaga H, Hashimoto H, Horiguchi H, et al. Variation in cancer surgical outcomes associated with physician and nurse staffing: a retrospective observational study using the Japanese Diagnosis Procedure Combination Database. BMC Health Serv Res 2012;12:129. [Crossref] [PubMed]
- Chung W, Sohn M. The Impact of Nurse Staffing on In-Hospital Mortality of Stroke Patients in Korea. J Cardiovasc Nurs 2018;33:47-54. [Crossref] [PubMed]
- Lee JE, Kim TH, Cho KH, et al. The association between number of doctors per bed and readmission of elderly patients with pneumonia in South Korea. BMC Health Serv Res 2017;17:393. [Crossref] [PubMed]
- Jagsi R, Weinstein DF, Shapiro J, et al. The Accreditation Council for Graduate Medical Education's limits on residents' work hours and patient safety. A study of resident experiences and perceptions before and after hours reductions. Arch Intern Med 2008;168:493-500. [Crossref] [PubMed]
- Needleman J, Buerhaus P, Pankratz VS, et al. Nurse staffing and inpatient hospital mortality. N Engl J Med 2011;364:1037-45. [Crossref] [PubMed]
- Michtalik HJ, Yeh HC, Pronovost PJ, et al. Impact of attending physician workload on patient care: a survey of hospitalists. JAMA Intern Med 2013;173:375-7. [Crossref] [PubMed]
- Pronovost PJ, Angus DC, Dorman T, et al. Physician staffing patterns and clinical outcomes in critically ill patients: a systematic review. JAMA 2002;288:2151-62. [Crossref] [PubMed]
- Patout M, Sesé L, Gille T, Coiffard B, et al. Does training respiratory physicians in clinical respiratory physiology and interpretation of pulmonary function tests improve core knowledge? Thorax 2018;73:78-81. [Crossref] [PubMed]
- Qiao R, Rosen MJ, Chen R, et al. Establishing pulmonary and critical care medicine as a subspecialty in China: joint statement of the Chinese thoracic society and the American college of chest physicians. Chest 2014;145:27-9. [Crossref] [PubMed]
- Qiao R, Marciniuk D, Augustyn N, et al. Establishing Pulmonary and Critical Care Medicine in China: 2016 Report on Implementation and Government Recognition: Joint Statement of the Chinese Association of Chest Physicians and the American College of Chest Physicians. Chest 2016;150:279-82. [Crossref] [PubMed]
Cite this article as: Jiang J, He R, Yin H, Li S, Li Y, Liu Y, Qiu F, Hu C. Respiratory healthcare resource allocation in rural hospitals in Hunan, China: a cross-sectional survey. J Xiangya Med 2020;5:4.


