
Huge mediastinal teratoma in children: anesthesiological approach, surgical strategy and literature review
Introduction
A teratoma is a germ cell tumor derived from pluripotent cells composed of complex differentiated tissues comprising elements of more than one embryonic cell layers: ectoderm, endoderm, and mesoderm (1-3). The incidence of teratoma is around 1 in 4,000 live births (3). We observe, in paediatric age group, that mediastinal localisation is rare (about 1–3% of all the germ cell neoplasms) (3). In practice, mediastinal mass syndrome in children presents a common dilemma as far as the management techniques and surgical approach are concerned. Our present case is specific in its clinical presentation and approach, requiring multidisciplinary care in order to obtain a successful strategy in the excision of a mediastinal tumor, following an anterior emergency thoracotomy issuing in an uneventful recovery.
Case presentation
The patient was a baby girl aged 5 months presented with history of recurrently productive cough and dyspnea with haemoptysis for at least one month. During the medical history, pregnancy had been normal and she was delivered at full term though treated with steroids during each episode of pulmonary tuberculosis. She was admitted to the emergency for a low-grade fever, cough and breathlessness.
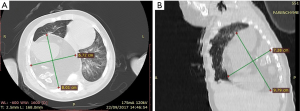
Physical examination showed no external abnormalities, although, during respiration, we could observe some chest indrawing located in the lower intercostals spaces. The auscultation found decreased air entry on the right side in infraclavicular. The percussion of the chest revealed a generalized dullness of the right hemithorax. Laboratory findings were normal except low haemoglobin level (7.7 g/dL). Serum levels of α-factor protein and β-HCG values were normal. A chest X-ray showed a large intrathoracic homogenous opacity with calcification in the mediastinum and the right hemithorax. The heart was markedly displaced to the left. Contrast-enhanced CT of the thorax revealed a well-defined hypo-dense mass, heterogeneously enhanced, measuring 8.01×6.72×7.28 cm3, with multiple areas of fat density and multiple calcification in the anterior mediastinum extending into the right pleural cavity (Figure 1). The mass was causing compression on the right main bronchus and displacing the mediastinal structures. The patient was admitted immediately to the surgical emergency for complete resection. She underwent a right anterolateral thoracotomy through the 5th intercostal space. A tumor was visible immediately when the pleura was opened. Intraoperatively, a large mass of 12 cm × 10 cm × 8 cm occupied nearly the entire right hemithorax, and was partly solid, partly cystic. A 50 cc syringe is used to aspirate the fluid part to decrease the tumor’s volume and facilitate the extirpability of the mass. The adherence to the anterolateral chest wall and the right lung complicated the dissection all around the tumor. The mass was dissected and was resected completely without hemorrhagic incident on vital organs (Figure 2A). Postoperative period was uneventful (Figure 2B). Chest drain was removed on the 5th postoperative day and she was discharged on the 7th postoperative day, following a chest X-ray revealing a complete lung expansion. No recurrence was noted in 2 years follow-up. A microscopy of the resected specimen confirmed a mature teratoma presenting cystic structures lined with stratified squamous epithelium, furthermore, at places, cartilage, bone, respiratory epithelium, mucous secreting glands, adipose tissue, and vessel tissue were located. No malignant or immature component was found.

Discussion
The word Teratoma is derived from Greek words “terato” meaning monster and “onkoma” meaning “monster” and “swelling,” respectively (2,3). Teratomas of the anterior mediastinum are uncommon and comprise 1% to 5% of all mediastinal tumours (4). The average age of onset is between the second and third decades of life without gender prediction (3,5). Our case however deals with a teratoma discovered early in a baby aged 5 months following a rare and alarming symptomatology including haemoptysis and recurrent respiratory infection, justifying systematic overview of the tips and tricks management of this mediastinal lesion.
Anesthesiological approach
Mediastinal masses required particular anesthetic considerations. It is important to determine the position of the patient before surgery of mediastinal mass to avoid complications related to compression of vital intra mediastinal organs. The positional changes preoperatively, intraoperatively or postoperatively can increase the risk of life-threatening due to respiratory compromise and cardio-vascular compression, causing airway reduction and cardiac tamponade due to drop in central venous pressure (6,7).
In order to establish the anesthesiological classification risk of the patient, preoperative evaluation and risk assessment includes (Table 1) (8-10):
Table 1
| Grade | Category | Symptomatology | CT scan = tracheobronchial obstruction |
|---|---|---|---|
| Safe | Adult | Asymptomatic | <50% |
| Unsafe | Adult or child | Severely*** symptomatic | – |
| Child | Regardless of symptoms | >50% | |
| Uncertain | Child | Mild*/moderate** symptomatic | <50% |
| Adult | Mild/moderate symptomatic | >50% | |
| Adult or child | Unable to give history | – |
*, mild: can lie supine with some cough/pressure sensation; **, moderate: can lie supine for short periods but not indefinitely; ***, severe: cannot tolerate supine position.
- A well guided physical examination;
- Radiological evaluation (CT scan and chest X-ray) for sizing of the mediastinal mass and to evaluate the repercussions on the cardio-respiratory functions;
- Awake fiberoptic evaluation of the tracheobronchial tree for evidence of severe extrinsic compression;
- Multivariate analysis which revealed that pulmonary function testing (PFT) mixing obstructive and restrictive pattern on PFT predicted a greater rate of postoperative cardiorespiratory compromises;
- Positional echocardiography to determine the degree of tracheal or bronchial compression.
Using logistic regression analysis to identify the factors associated with anesthetic complications, a study was conducted over 118 children presenting mediastinal masses in which Anghelescu et al. (11) demonstrated that orthopnea, compression of a main stem bronchus, upper body edema, and great vessel occlusion were all statistically significant. Bussières et al. could fix a threshold value of more than 130 cm3 of the mediastinal mass, predisposing to an increased risk of postoperative complications (12).
In preoperative period, the anesthesiologist may be prepared and can anticipate (6):
- An emergency extracorporeal circulation (CEC) or ECMO cannulation for airway obstruction >50%, to prevent tracheomalacia and peri- and postoperative complications.
- A large-bore femoral venous access line either in the case of an superior vena cava (SVC) syndrome, or in the case when surgery may involve clamping or resection of the SVC intraoperatively.
- Anesthesiology literature reports that, anaesthesia with inhalation agents and short-acting medications or local and regional anaesthesic techniques with sedation should be widely employed for high-risk patients and maintained either with spontaneous ventilation via an endotracheal tube or facemask or laryngeal mask airway, or with jet ventilation while achieving a surgical level of anesthesia (7,8,13).
The use of helium-oxygen mixtures (Heliox®) have been recommended in patients with severe tracheobronchial obstruction or compression to promote laminar gas flow (13).
Blank et al. recommend tracheal intubation without neuromuscular blockade and safely positive-pressure ventilation after sternotomy decompression of the mediastinum to avoid the cardiorespiratory compromises. According to them, the intravenous agents as dexmedetomidine and ketamine, are useful in this context as they have analgesic and sedative properties with minimal respiratory depression (14).
During the intraoperative period, an acute hypoxemia due to the airway obstruction or to the compression, require, in descending order (9,15):
- Awake fiberoptic scope to help to control intubation position if obstructing mass is proximal on CT scan (tracheal localisation). In our case, double lumen ventilation with right sided endotracheal tube is mandatory to give surgeons easy control and dissection of the mass;
- Re-positioning of the patient in “Rescue” position to displace the mass and reduce its pressure on the airway or venous return;
- If obstruction or compression or collapse is distal (carina, and/or bronchi), airway or bronchi desobstruction with rigid bronchoscopy is necessary. Moreover, a new intubation with an endotracheal tube having an appropriate size is reinforced beyond the site of obstruction;
- Preparation for resuscitation thoracotomy;
- In the postoperative period, awake extubation for the patient is recommended, in a sitting position, and the patient is monitored during twenty-four hours to reduce the complications related to the postoperative edema of the pathologic surrounding tissues (9).
Surgical strategy
The first step to undertake in the evaluation of the surgical risk is the use of CT to clearly identify the localization, the size, the density, the contents, the structure of the mass (calcification) and its adherence to important structures.
The second surgical evaluation step is proceeded to:
- Develop a list of differential diagnoses of the masses, because of similarities in the X-ray images such as that of an anterior mediastinal mass in neonate including congenital cystic adenomatoid malformation, pulmonary sequestration, intrapericardial teratoma, and cardiac rhabdomyosarcoma;
- Identify a compression and invasion signs located in the tracheobronchial tree, in the pulmonary vascular structures, the superior vena cava and other mediastinal vascular structures or in the vertebrae;
- Discuss about the tumor resectability;
- Identify and prevent a potential medical morbidity.
The purpose of the surgery of the mass mediastinal is to establish the diagnosis and prevent life-threatening complications caused by the airway and hemodynamic compromise. Planning surgery is mainly reliant to CT scan. It demonstrates the extent of the mass (tumour size, location, expansion) (3) and defines the appropriate operative procedure which depends on the background of the patient such as his age, the patient’s history of symptoms, co-existent morbidity, the cardiorespiratory endurance on the one hand and on the other hand, the surgeon’s experience is also of an appreciable advantage.
Dealing with the surgical approaches, the literature reports have described approaches of mediastinal tumour excision with median sternotomy (15), anterolateral thoracotomy, posterolateral thoracotomy, clamshell incision (5). In our opinion, the best and adequate surgical procedure for an anterior mediastinal mass is the one that permits safe dissection.
The main difficulty encountered in the surgery of a mediastinal teratoma is its involvement of vital structures. Surgical maneuvers are always complicated by the inflammatory strong adhesions and the erosion of surrounding mediastinal structures due to proteolytic or digestive enzymes produced by the teratoma (1,15).
In our case, we advocate for an anterolateral thoracotomy, which can be transformed into a ‘trapdoor’ incision or clamshell incision, enabling an adequate exposure to access both the pleural cavity and the hilar structures for a safe removal. Some authors report a successful removal for smaller mediastinal teratoma with video-assisted thoracoscopic surgery techniques (1,5). The surgeon should always be ready and figure out that the incision should be extended or modified in the case where an additional exposure is required. Other surgical procedures must be anticipated such as lung wedge resection, lobectomy or prosthetic vascular and pericardial reconstruction as GORE® PRECLUDE® (0.1 mm) patch if a strong adherence occurs (1).
Conclusions
Mature teratoma should be considered in aetiological diagnosis of haemoptysis in children. Complete resection is curative for germ cell tumours and is the mainstay of treatment for them with a safe outcome for the patient. A multidisciplinary management including anesthesiologist, intensivist, thoracic and paediatric surgeon is necessary to provide tailored preoperative care for each individual patient, based on clinical, radiological and functional evaluation of the risks, as well as any other data to prevent or manage cardiorespiratory complications. Appropriate pre-surgical planning, positioning of the patient, approach of the incision, exposure, associated with intraoperative relevant decisions are all the keys to successful resection.
Acknowledgments
We would like to thank Andriantsiory Esteban Razafimanjato for his help to publish this paper.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.08.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Pattnaik MK, Majhi PC, Nayak AK, et al. A rare presentation of a huge mature mediastinal teratoma with right lung cavitation. BMJ Case Rep 2014; [Crossref] [PubMed]
- Anand S, Longia S, Agarwal N, et al. Mature Mediastinal Teratoma-A Rare Cause of Recurrent Respiratory Distress. People’s Journal of Scientific Research 2010;3:33-5.
- Dhond AP, Agrawal SO, Sirmukaddam SV, et al. Mediastinal teratoma: A case report with review of literature. J Sci Soc 2016;43:57-9.
- Starer F. The successful removal of an anterior mediastinal teratoma from an infant. Arch Dis Child 1952;27:371-4. [Crossref] [PubMed]
- Liew WX, Lam HY, Narasimman S, et al. Mediastinal mature teratoma in a child- A case report. Med J Malaysia 2016;71:32-4. [PubMed]
- Li WW, van Boven WJ, Annema JT, et al. Management of large mediastinal masses: surgical and anesthesiological considerations. J Thorac Dis 2016;8:E175-84. [Crossref] [PubMed]
- Erdös G, Tzanova I. Perioperative anaesthetic management of mediastinal mass in adults. Eur J Anaesthesiol 2009;26:627-32. [Crossref] [PubMed]
- Datt V, Tempe DK. Airway management in patients with mediastinal masses. Indian J Anaesth 2005;49:344-52.
- Martinovsky P, Swanevelder J. Anesthésie pour médiastinoscopie chez les patients ayant une masse médiastinale. Le praticien en anesthésie réanimation 2008;12:422-8.
- Béchard P, Létourneau L, Lacasse Y, et al. Perioperative cardiorespiratory complications in adults with mediastinal mass: incidence and risk factors. Anesthesiology 2004;100:826-34; discussion 5A.
- Anghelescu DL, Burgoyne LL, Liu T, et al. Clinical and diagnostic imaging findings predict anesthetic complications in children presenting with malignant mediastinal masses. Paediatr Anaesth 2007;17:1090-8. [PubMed]
- Bussières J, Leone M. Anesthésie-réanimation en chirurgie thoracique. John Libbey Eurotext, 2017.
- Galway U, Doyle DJ, Gildea T. Anesthesia for endoscopic palliative management of a patient with a large anterior mediastinal mass. J Clin Anesth 2009;21:150-1. [Crossref] [PubMed]
- Blank RS, de Souza DG. Anesthetic management of patients with an anterior mediastinal mass: continuing professional development. Can J Anaesth 2011;58:853-9, 860-7. [Crossref] [PubMed]
- Garey CL, Laituri CA, Valusek PA, et al. Management of anterior mediastinal masses in children. Eur J Pediatr Surg 2011;21:310-3. [Crossref] [PubMed]
Cite this article as: Razafimanjato NNM, Rajaoharimalala TG, Abdou Rabi R, Ravoatrarilandy M, Rajaonera AT, Hunald FA, Rakotovao HJL. Huge mediastinal teratoma in children: anesthesiological approach, surgical strategy and literature review. J Xiangya Med 2019;4:35.


