Cardiovascular diseases in Tanzania: The burden of modifiable and intermediate risk factors
Background information
The magnitude of non-communicable diseases (NCDs) is increasing all over the world in unmanageable scale. There is a disproportionate higher burden of cardiovascular diseases (CVDs) and their associated risk factors in many part Sub-Saharan countries. Lack of appropriate epidemiological data (1), coexistence of infectious and non-infectious diseases, under-nutrition/over-nutrition, and poor economic status are among the factors that influence CVDs mortality in these countries (2,3). CVDs mortality is expected to rise from 17.9 million deaths to 23 million deaths from 2015 to 2030 if no appropriate measures are taken to alleviate the problem (3,4). Low and middle-income countries (LMICs) are experiencing a higher burden of CVD deaths due to rapid urbanization, aging, health and nutrition transitions (4). Treatment and management of CVDs and their associated risk factors depend much on capacity of the countries to utilize the available resources in the prevention and control of the diseases (5). Furthermore, higher costs for diagnosis, treatment, and management of CVDs influence the increased CVDs premature deaths among the most productive individuals (<70 years) in the world (6). This has contributed to the increased number of patients (inpatients and outpatients) in hospital settings all over the world (7).
In 2013, more than one billion people in sub-Saharan countries, including Tanzania, were affected by CVDs. The disease is accounting for 38.3% of all NCDs deaths, 11.3% of deaths from all causes in the region and 5.5% of the global CVD-related deaths (4). Cardiovascular-related diseases are expected to double in sub-Saharan Africa (SSA) by 2020 if there will be no implementation of preventive measures (8). According to Global Burden of Diseases, Injuries and Risk Factors 2010 Study, the most common leading cause of CVDs deaths in Sub-Saharan region were: stoke (38.8%), ischemic heart diseases (28.6%), hypertensive heart diseases (7.0%) and peripheral artery diseases (0.3%) (2). Similarly, hypertensive heart disease (41%), valvular heart diseases (18%), coronary heart diseases (18%), peripartum cardiomyopathy (7%), non-hypertensive dilated cardiomyopathies (6%) in adults, and congenital heart disease (34%) in children were the most leading cardiovascular-related diseases in Tanzania between 2015–2017 (9). The incidence of CVD mortality in SSA increased to 81% from 1990 to 2013, with higher death rates in women (512,269) than in men (445,445), and with more deaths from stroke than ischemic heart diseases 409,840 and 258,939, respectively (4).
Trends of CVD death rates in SSA, including Tanzania, are highly driven by lifestyles changes, characterized by low levels of physical activity, excessive alcohol consumption, tobacco use and unhealthy eating (10). Poor management of these factors has resulted into intermediate risk factors such as raised blood pressure, raised blood cholesterol, diabetes, overweight and obesity, that have direct linkage with CVDs (11). All these factors occur as a result of rapid urbanization, modernization, socio-economic status and increased advertisement of Westernized food market (8,12). Despite the increased trends of CVDs, the burden of the associated risk factors is not well known, especially in Tanzania. The focus of this review is to summarize the current situation of CVDs in Tanzania, including the associated risk factors and status of primary health care in the control and management of CVDs.
Current situation of CVDs in Tanzania
Tanzania like other developing countries is experiencing a higher burden of NCDs, with CVDs being the most prevalent diseases among the NCDs. According to recent estimates, approximately 33% of all Tanzanian population is affected by NCDs, mainly CVDs, cancer, diabetes and chronic respiratory diseases (12). The probability of dying from NCDs among adults aged 30 to 70 years is approximated to 16% (13,14). Cardiovascular diseases alone are responsible for 13% of the total NCDs deaths in Tanzania and adults aged 25–64 years are highly affected (12). Age-standardized CVDs mortality rates showed higher death rates among Tanzanian men compared to women (473 versus 382 per 10,000 population) (10). There an increased prevalence of CVDs deaths rates from 9–13% between 2012 and 2016 in the country (12,13), and these has been driven by the growing trends of CVD risk factors in the country (10). If no strategic measures are taken, the rates of CVD mortality-related diseases in Tanzania are expected to rise by 20% in 2020, and this will cause over one million deaths (14).
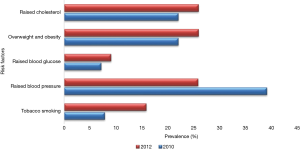
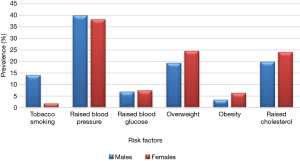
In order to ensure actual control and management of NCDs, the government of Tanzania has developed and implemented the national strategic plan 2009–2015 that included different stakeholders for a unified action to fight against NCDs including CVDs. This has been done through improvement of healthcare system that includes provision of improved prevention methods, realistic diagnostic equipment, and affordable treatments (14). The government of Tanzania has created favorable environment through provision of improved and valuable healthcare services to all individuals suffering from NCDs (14). However, despite these efforts, subnational STEP survey conducted in 2012 showed higher prevalence of CVDs and their associated risk factors (Figure 1) both in men and women as depicted in Figure 2 (10, 13). The rise of CVD risk factors has been attributed to high costs of healthcare services, untrained health workers, lifestyle modifications, negative effects of globalization, urbanization and migration of rural dwellers to urban areas (15).
Risk factors for developing CVDs
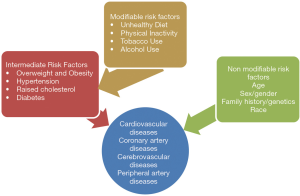
Among types of NCDs, CVDs are number one causes of deaths in Tanzania (10,13). CVDs share similar risk factors with other NCDs as shown in Figure 3. Intermediate risk factors like overweight and obesity, hypertension, diabetes, and hyperlipidemia present in individuals as a result of poor management of behavioral risk factors (12).
Modifiable risk factors
Modifiable/behavioral risk factors are most common preventable risk factors that underlie the development of CVDs. These include unhealthy eating, tobacco use, excessive alcohol intake, and physical inactivity. Poor management and prevention of these risk factors leads to metabolic/physiological changes that accelerate to the development of CVDs.
Excessive alcohol use
Alcohol consumption has been associated with increased CVDs risks, such as raised blood cholesterol, high blood pressure, platelet coagulation and increased fibrinolysis (16). Alcohol consumption is also related to increased risk of atrial fibrillation (an abnormal cardiac rhythm), cardiomyopathy, acute myocardial infarction, hemorrhagic stroke and ischemic stroke (17). Globally, the amount of pure alcohol consumed by a person aged ≥15 years were estimated to 6.2 liters/person in 2010 (16). An average pure alcohol consumption were estimated to be 7.7 liters per person aged ≥15 years (average of 11.4L from males and 4.0L from females in Tanzania (16). The most common types of alcohol beverages consumed in Tanzania are as summarized in Figure 4 (16).
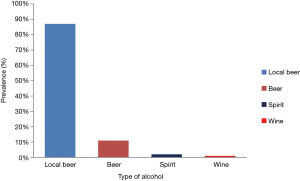
In 2012, prevalence of alcohol consumption among men and women in Tanzania were reported to range from 23–38% and 13–13%, respectively (10). Further results showed that 29.4% (38.3% men and 20.9% women) of the adult population were current alcohol users. Among them, 27.4% of men and 13.4% of women were binge drinkers (10). Moreover, 17.2% of adults aged 15–59 years were reported as current alcohol users in urban settings, and this was associated with socio-economic status of urban dwellers (18).
Some of the chronic diseases such as hypertension, kidney diseases (10) and diabetes (19) are increasing in Tanzania due to high number of alcohol drinkers. Higher prevalence of hypertension (50%) was reported among alcohol users compared to non-alcohol users (49.3%) in a study conducted in Mafia Island (18). Furthermore, alcohol consumption was related to increased CVD risk factors, such as diabetes (9.8%) hypertension (53.3%), overweight and obesity (73.3%) among study participants (19). There is a growing rate of alcohol consumption among Tanzanian population that has been related with the increased NCDs and other alcohol related-diseases, including breast and liver cancers, despite enforcement of alcohol policy in the country (16,17). Legal binding regulations on alcohol advertisement and sponsorship should therefore be effectively and efficiently implemented, in order to lower the increased trends of alcohol users and alcohol-related diseases, which later accounts for higher costs of treatment and management.
Unhealthy diets
Diet plays an essential role in the etiology and pathophysiology of different CVDs. Diet and nutrition have been recognized as major contributors atherosclerotic plaque formation and development of CVDs, including CHD and stroke. Unhealthy diet is linked to other CVD risk factors such as high blood pressure, elevated blood cholesterol, diabetes, overweight and obesity (20). According to subnational STEP survey [2012], only 9.2% of individuals aged 25–64 years in Tanzania consumed at least less than 5 servings of fruits or vegetables on average per day (10). Although there is only one current national data on dietary patterns, scientists have still reported the influence of dietary intake on etiology and pathophysiology of CVDs (21-24). Knowledge on food choices plays a crucial role in the etiology of CVDs, and adoption of a healthy diet can subsequently reduce CVD risk like hypertension and hyperlipidemia (22,23). Dietary changes can greatly contribute to changes in mean body mass index (BMI), total serum cholesterol, and increased levels of blood pressure (23). Diet with trans-fats and saturated fat increases risks for CHD, while a diet rich in polyunsaturated fats reduces CVD risks (22,23). A study conducted in peri-urban Tanzania revealed the association between use of palm oil as cooking oil, inadequate consumption of fruits and vegetables and high intake of meat with increased blood cholesterol (22). Higher prevalence of hypertension in urban areas, especially among women, has been related to higher consumption of meat and coconut oils (23). Moreover, higher consumption of protein-rich foods, particularly meat, milk and blood with an inadequate intake of fruits and vegetables were associated with increased risk of hypertension among Maasai living in Simanjiro district (24).
Higher consumption of highly processed foods, dietary salt (23,24) with low levels of physical activity, and low knowledge of dietary choices were associated with increased prevalence of hypertension in different settings of Tanzania. Higher intake of fruits and vegetables is well known to alleviate CVD risk factors, due to higher contents of vitamins and nutrients like vitamin C, vitamin A, vitamin B, potassium (K), Magnesium (Mg) and Calcium (Ca). However, different studies conducted in the country reported low consumption of fruits and vegetables among Tanzanian population (10,22). Healthy eating that includes at least five serving of fruits and vegetables per day, low salt intake and animal foods can all help to prevent some CVDs like heart attack and stroke (24). Dietary intervention should therefore focus on provision of nutrition education to raise awareness on healthy dietary choices and dietary diversity to the general population.
Physical inactivity
Each year, physical inactivity contributes to approximately 3.2 million deaths worldwide (25,26). Physically inactive people have 20% to 30% increased risk of all-cause mortality due to NCDs (27). People who engage in regular physical activity have reduced risk for CVD, overweight, obesity, hypertension, diabetes, depression and some cancers, including breast and colon cancer (19,28-30). Women and elderly, especially those suffering from chronic illnesses, such as arthritis and osteoporosis, are more likely to be less active than men and younger people (26,31). Majority of Tanzanian population (97%) involved in the national STEP survey [2012] met the WHO-recommended levels of physical activity, 98% of them being in the rural and 92% in the urban population (10).
Moreover, urban settings represent low levels of physical activity compared to rural areas, due to sedentary lifestyles and subsequently urban population faces higher incidence of overweight, obesity, and elevated blood cholesterol levels than rural population (29,30). Approximately 21% of men in rural and 96% of women in the urban population of Tanzania were reported to have no regular physical activities in a population-based cross-sectional survey for NCDs (32), and this might be due to sedentary lifestyle among urban dwellers as compared to manual activities performed by rural dwellers. Another prospective cohort study conducted in Tanzania showed that migration from rural to urban areas reduced the level of physical activity by 52.9% (79.4% to 26.5%) in men and 21.9% (37.8% to 15.6%) in women (28). Low levels of physical activity have been associated with increased body weight, diabetes, unfavorable lipid patterns and other CVD risk factors in rural and urban settings of Tanzania (28,30).
Tobacco use
Worldwide, nearly one billion peoples are current smokers (30), with more than 7 people dying each year from smoking-related diseases (33). Of all deaths occurred in 2010, six million deaths resulted from direct smokers and 890,000 deaths were from non-smoker/second-hand smokers (30,33). Annual tobacco-related deaths are anticipated to rise to 8 million by 2030 according to WHO estimates, and it is expected to cause 10% of all deaths globally if no appropriate measures will be taken to stop smoking (26). Moreover, more than three-quarter of smokers live in low and middle-income countries where the burden of tobacco-related diseases and deaths is also high (33,34). According to TDHS 2015/16 tobacco smoking is most common in men (14%) than in women (1%), and among men who smoke daily, 41% smoke <5 cigarettes/day and 30% smoke 5–9 cigarettes/day (35). The prevalence of tobacco and cigarette smoking among adults in Tanzania is 14.1% (29.0 in males and 2.9% in females) for current tobacco smokers, 11.8% for daily tobacco smokers and 9.4% for daily cigarette smokers (34). Currently, there is no much information concerning the use of tobacco in Tanzania, however, few studies have documented higher incidence of tobacco use among men and women. Latest national STEP survey [2012] showed that 28% of male use tobacco and 15.9% of adults aged 25–64 years were current smokers (10). Another study by Kapito-Tembo (36), showed that, approximately 21% of the study participants were tobacco users, with 19% cigarette smokers, 45% using other forms of tobacco (snuff and chewing tobacco) and over 15% using pipes.
The prevalence of tobacco and cigarette smokers in Tanzania increased from 7.9% to 15.2% from 2008 to 2012 (21,37). Smoking is a major contributor of CVDs and other chronic illnesses that lead to airway diseases like pneumonia, emphysema and chronic bronchitis, and also lung cancer. Smoke-related diseases are higher in Tanzanian men than women (37). For example, the prevalence of hypertension was observed to be higher (52%) among smokers compared to non-smoker (26.1%) in a study conducted in Dar es Salaam (38). A study conducted in Tanzania by Kidane et al., [2015] (37) reported high prevalence of smoking-related diseases among men (41.3%) and women (8.5%), respectively. Further results showed that males participants were 1.8 times more likely to be smokers compared to females and the rate of smoking in men increased with age from 1% at the age of 15–19 years to 31% at the age of 45–49 years (37). In Tanzanian population, smoking prevalence varies from one part of the country to another. Cigarette smoking is very common in Southern zone (31%) while the Southern Highlands (12%) has the least smoking prevalence, this being highly influenced by the low level of education and poor economic status (38).
Moreover, most smokers in Tanzania seem to lack enough knowledge on health consequences of smoking and their corresponding higher health cost, and reduced incomes that are derived from smoking-related diseases (37). Health education programs on smoking and tobacco use and their health impacts should therefore be well integrated into the school and health center. On the other hand, Tanzanian government ratified the WHO framework convention on tobacco control in 2007, with the purpose of providing education and sensitizing parliament members on changing their perception that tobacco was vital for the country’s economy, including awareness education on negative health effects of cigarette smoking, by looking into health effects and related cost of treating smoking-related diseases. Youth under 18 years and non-smokers have been protected by youth legislation on tobacco control and through the establishment of a smoke-free environment to all public places (39). However, tobacco use, particularly among the youths, is aggravated by increased advertisement, promotion, and sponsorship of tobacco products by tobacco industries.
Intermediate risk factors
Intermediate risk factors have a direct link with NCDs (26), as they appear as a result of uncontrolled behavioral risk factors. Key intermediate risk factors for CVDs include: raised blood pressure, diabetes, raised blood cholesterol, overweight and obesity.
Hypertension
Hypertension is one of the leading risk factors for global mortality (accounting for 13% of the total deaths) (40), attributing to more than 45% of all CHD deaths and 51% deaths due to stoke (41). Hypertension is affecting more of the population in low and middle-income countries in which health systems are also weak (3). Prevalence of hypertension is increasing in the African region, with 45% of adult people aged ≥25 years suffering from high blood pressure (41). Uncontrolled blood pressure can result in more health complications, such as heart diseases, renal diseases (42), diabetes, myocardial infarction, aneurysms, stroke, impaired insulin activities, premature mortality and morbidity (41).
According to WHO country profile report for NCDs [2014], approximately 31.6% of men and 29.4% of women in Tanzania were hypertensive, and the probability of dying from the four main types of NCDs, including hypertension and other CVDs, were estimated to be 16% (13) .Moreover, there is a rapid increase on the prevalence of hypertension in Tanzania, with significant variation in rural and urban settings that is characterized by sedentary lifestyles, urbanization and aging population (43,44) as reviewed above. From 1996–1997, prevalence of hypertension was found to range from 19–35% in rural and urban settings (13). However, the prevalence has been shown to rise from 2–10% in 1960s to 13–79% in 2016s in rural and urban Tanzanian population, with inadequate control response (45). Approximately 33% of men and 32% of women living in rural areas are regarded as hypertensive compared to 30% and 28.6% among men and women in urban areas, respectively (46).
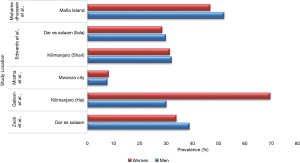
Moreover, hypertension and hypertension-related diseases have been reported as one of the leading cause of hospital admissions and mortality rate in Tanzania. Hypertension was the main cause of deaths in a 3-year prospective study conducted at Bugando hospital, accounting for 34% of all NCDs deaths and 15% of overall deaths. Hypertension was the leading cause of death among patients aged ≥50 years, and more than 50% of hypertension-related deaths occur before retirement age (42). Results from prospective observational study conducted at the Cardiovascular Center of Muhimbili National Hospital in Dar es Salaam showed that, 45% of the heart failure patients were hypertensive (47). Despite a higher prevalence of hypertension in different areas of Tanzania, many people are not aware of the related risk factors, with low rate of diagnosis and treatment. Table 1 shows a summary of the status of awareness and control of hypertension in Tanzania. The increased prevalence of hypertension (Figure 5) in Tanzania demonstrates a need for cost-effective strategies, including primary prevention, timely treatment, and effective blood pressure control measures. All this will reduce the growing CVDs burden in the country, and hence improve the overall health and well-being of individuals, by reducing costs of treatment and management of other related chronic diseases.
Table 1
| Region | Awareness | Undiagnosed/untreated | Treated | Reference |
|---|---|---|---|---|
| Dar es Salaam | 48% | – | 22% | Zack et al., (48) |
| Kilimanjao (Hai) | 48.3% | 95.3% | 23% | Galson et al., 2017 (49) |
| Mwanza city | 9.4% | Male (4.1%), female (8.5%) | 7.1% | Mosha et al., 2017 (50) |
| Kilimanjaro (Shari) | 32% | – | 22% | Edwards et al., (46) |
| Dar es Salaam (Illala) | 18% | 0.7% | 10% | Edwards et al., (46) |
| Mafia Island | 26.6% | 79.4% | 20.6%, 57.6% | Muhamedhussein et al., (18) |
Raised cholesterol
It is known that raised blood cholesterol is a common risk factor for CVDs, including ischemic heart diseases, stroke and heart failure (48). In 2008, 38% of the world population had higher levels of blood cholesterol (30). Prevalence of raised blood cholesterol was highest (54%) in WHO European region and lowest (23%) in the WHO African region (40). This was influenced by sedentary lifestyles and rapid urbanization in these countries. Nearly 20% of males and 24% of females in Tanzania had higher blood cholesterol >5 mmol/L according to WHO estimates in 2010 (45). Kilimanjaro region have been reported with highest prevalence of raised cholesterol (17.4% of men and 19% of women) compared to other regions of Tanzania like Morogoro (5% of men and 6.7% of women) and Mara (4.8% of men and 6.9% of women) (51). Njelekela et al., [2009], reported higher prevalence (48%) of serum triglyceride among study participants, and were associated with higher prevalence of overweight (33%) obesity (23%) and hypertension (57%) (52). Another recent study conducted in Dar es Salaam showed that, 37% and 45% of men and women who participated in the study had serum total cholesterol (TC) of ≥200 mg/dL (22).
Furthermore, poor dietary diversification contributes to increased blood cholesterol. Lower intake of fruits and vegetables and higher intake of red meat have been linked to increased levels of blood cholesterol (23). For example, higher intakes of coconut oil, palm oil, and meat showed an association with increased blood cholesterol (29). Shifting from using saturated to unsaturated oil and encouraging people to eat at least five servings of fruits and vegetables per day can help to reduce blood cholesterol and CVDs.
Diabetes
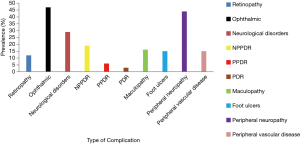
Diabetes is a growing public health problem that presents high cost for its control and management by the society. Globally, in 2014 approximately 9% (11% of men and 15% of women) adults aged ≥18 years were suffering from diabetes (27). Diabetes is causing 6% of the global deaths, with 83% occurring in low and middle-income countries (27). Furthermore, diabetes is attributed in causing more than 22% and 16% deaths worldwide, due to coronary heart diseases and stroke, respectively (40). Prevalence of diabetes varies from one region to another and this depends on the availability and country capacity to utilize the available few resources in prevention and management of diabetic cases (53). According to International Diabetes Federation [2017] estimates, more than 1.7 million people living in Sub-Saharan region are diabetic and Tanzania has been mentioned as among the country with the highest prevalence of diabetes (54). Results from the current national survey [2012] showed that more than 9% (8% of men and 10% of women) of adult population aged ≥25 years were diabetic (10), while the previous study reported lower prevalence of diabetes (2%) in rural settings of Tanzania (54). Moreover, recent findings showed higher prevalence of diabetes (up to 21.7%) in the rural population (19). Higher prevalence of diabetes is highly driven by rapid urbanization, sedentary lifestyles, and nutrition transition, which later emerge in the community as overweight and obesity (55,56). This pose another health challenges to the community members when seeking diabetic care in healthcare facilities. In addition, lack of diabetes guidelines, screening tools, poor reporting system, inadequate drug therapy and lack of training among healthcare providers and beneficiaries have been found to be potential reasons as to why many dispensaries and healthcare centers fail to provide valuable diabetic care in Tanzania (55-57). All these leads to the increased diabetic complications (angina, myocardial infarction, stroke, peripheral artery disease, and congestive heart failure), which account to 50% of mortality and disabilities among diabetic patients (54), including other related complications, such as neuropathy, retinopathy, nephropathy and limb amputation (19). Figure 6 shows a summary of diabetic complications in Tanzania (19,58,59). Despite the growing trends of diabetes in Tanzania, still there is low rate of awareness on diabetes and its complications in the population (56). A study conducted in Mafia Island of Tanzania by Muhamedhussein (57) showed that only 30 patients were aware of having diabetes, and among the patients with known diabetes, only six (20%) had controlled random blood glucose. This information demands the need for primary prevention interventions, including diabetic screening program, education programs, and early detection of diabetes cases, for proper management, to minimize late-stage complications. There is also a need for continuous provision of healthcare education to diabetes patients in the country, in order to improve access to care and subsequent quality of life.
Overweight and obesity
Overweight and obesity are defined as a body mass index of ≥24.9 and ≥29.9 kg/m2, respectively (26). More than one-third (39%) of the world adult population aged 18 years and above were overweight in 2014, which were 38% for men and 40% for women, respectively (29). Furthermore, more than 1.5 billion of the adult populations were obese (11% of men and 15% of women). The likelihood of chronic diseases such as diabetes, hypertension, coronary artery diseases, strokes, cancer, obstructive sleep apnea and, osteoarthritis increases with increased body mass index (BMI ≥24.9 kg/m2) (29). According to WHO estimates, each year overweight and obesity contribute to more than 2.6 million deaths of the total global disease burden (30). Both socio-demographic characteristics and economic factors influence occurrence of overweight and obesity in the population (60). However, lack of enough statistics, together with socio-cultural beliefs, create greater challenges in understanding the trends of overweight and obesity as public health challenges in African countries, including Tanzania (60,61). Moreover, 22% of men and 26% of women aged ≥25 years were overweight and obese, according to WHO country 2011 profile report (26). Prevalence of overweight and obesity are still increasing in the country as reported in the STEPwise survey conducted in the country in 2012, which showed 26% of the adult population aged >25–64 years were overweight and obese, with women being more affected than men (37% of women versus 15% of men) (10). A study done in Dar es Salaam by Bovet and his colleagues (21) reported higher prevalence of overweight 28% in men and 27% in women, and obesity of 6.8% in men 7.4% among women. Findings from multi-country cross-sectional study conducted in 2016 in four SSA countries showed higher prevalence of overweight and obesity of 46% in rural Uganda, 48% in peri-urban Uganda, 68% in urban Nigeria, 75% in urban Tanzania and 85% in urban South Africa (62). Moreover, Shayo and Mugusi [2011] reported higher prevalence of obesity (19.2%) that was significantly more in women (24.7%) than in men (9%). Individual perception of body weight is one of the factors that contributes to the higher prevalence of overweight and obesity in Tanzania (60). For example, only 12% men and 25% women perceived their body weight as being obese as compared to overweight among individuals who participated in the study conducted by Muhihi et al., (63), and 22% men and 38% women perceived themselves as being overweight.
Few studies conducted in the country, especially in urban Der es Salaam, showed higher prevalence of overweight and obesity among school-age children. For example, another study by Mpembeni and colleagues (64) reported the prevalence of overweight and obesity of 15% (10.1% boys and 19.4% girls) among primary school children in Dar es Salaam, Tanzania. Further study results showed that only 1/3 (33.3%) of children perceived their body weight as being overweight and obese, and 35.4% had negative perception regarding their body weight (64). Despite the implementation of targeted educational programs regarding overweight and obesity, and their associated health consequences being highly recommended in Tanzania, especially in urban areas, there are still increased trends of overweight and obesity in the country. An appropriate perception of one’s own body weight is an essential element towards enhancement of body weight management, as it helps to instill self-consciousness behavior on weight control among adults and children in Tanzania.
Primary prevention of cardiovascular diseases in healthcare centers in Tanzania
The burden of CVDs can be prevented through early treatment and control of high risks, such as effective treatment and control of hypertension and diabetes. Tanzania, like other LMCs countries, is struggling to provide proper treatment and management of NCDs, including CVDs (65). Prevention of CVDs, however, is still receiving less attention in Tanzania, despite the rapid growth CVD risk factors as reviewed herein (10). For effective prevention and control of CVDs, different guidelines and strategies have been implemented through primary health care services for clinical CVD prevention and control, including the European Society of Cardiology (ESC) and World Health Organization (WHO) guidelines, all of which recommend medical prevention to all individuals based on consideration of single CVD risk factor (66). Primary prevention services should therefore particularly focus on conditions that are manageable and have larger impact on public health, by taking into consideration the availability of resources and capacity of healthcare systems in Tanzania (22). However, primary healthcare centers face many challenges, such as lack of skilled/qualified medical practitioners, which affect timely provision and appropriate treatment of CVDs, shortage of enough insulin and other CVD medications, geographical and financial constraints, as well as poor physical health condition of CVD patients (65).
Despite the fact that diabetic care services and management of hypertension are actively being improved in Tanzania, most of the people with diabetes, hypertension and low socioeconomic status are unable to receive continuous treatment (66). Moreover, most of the CVDs patients do not afford to buy their medicines at private pharmacies due to poverty, and this may contribute to the increased disease complications as reviewed herein (66). On the other hand, symptoms of diabetes, hypertension or other CVDs, such as blurred vision, muscle pain, and impaired memory, have contributed to the drop-out of patients from treatment schedules (19). Improvement of health care system therefore needs more consideration while dealing with reviewed challenges herein, including shortage of health services providers and allocation of resources.
Way forward
Despite reputable responses made by Tanzania towards control and management of CVDs, more efforts are still needed at country, regional and district levels, to increase the capacity for prevention, management, and control of CVDs (63). Comprehensive policies, such as tobacco/cigarette smoking policy, alcohol consumption policy, dietary policy, including labeling and marketing of food products, salt reduction policy, guidelines on clinical and nutritional management of CVDs, and physical activity, are essential elements in the management of CVDs in Tanzania (13). Moreover, primary prevention is an effective approach towards control of modifiable risk factors through implementation of different interventions, such as increased taxes on alcohol sales and prohibited use by under 18 years youths, cigarette smoking restrictions and reduction of population exposure to smoking. Other interventions should include raising awareness on fruits and vegetable consumption, and promotion of physical activity (67).
Finally, early detection and timely management of CVDs and their associated risk factors provide additional control measures, as late management and treatment of CVDs are proven to be costly, with higher mortality and morbidity (67). Community mobilization is also needed to implement prevention strategies to prevent exposure to CVD risk factors and subsequent reduction of the growing burden of CVDs.
Conclusions
Despite efforts taken by Tanzanian government in prevention and management of CVDs, there is still a growing trend of CVDs deaths and their associated risk factors in the general population. Higher prevalence of CVD risk factors highlights the need for early public interventions and adaptation of health care system, to meet WHO recommended standards. Mass campaigns/education on CVDs prevention for people at risks should therefore be well addressed in order to raise awareness to the community members. Encouraging community members to practice healthy eating, regular physical activity, to balance their energy expenditure as strategies for body weight management will help to reduce the burden of overweight and obesity, and therefore NCDs incidence in the country. Finally, the allocation of enough financial resources and integration of health sectors with all NCDs stakeholders will facilitate the management of CVDs and their associated risk factors.
Acknowledgments
The author wishes to thank Dr. Elingarami Sauli and Dr. Haikael David Martin (supervisors) for their invaluable support during the writing of this review.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.07.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Dalal S, Beunza JJ, Volmink J, et al. Non-communicable diseases in sub-Saharan Africa: What we know now. Int J Epidemiol 2011;40:885-901. [Crossref] [PubMed]
- Moran A, Forouzanfar M, Sampson U, et al. The epidemiology of cardiovascular diseases in sub-saharan Africa: The global burden of diseases, injuries and risk factors 2010 study. Prog Cardiovasc Dis 2013;56:234-9. [Crossref] [PubMed]
- Roth GA, Johnson C, Abajobir A, et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. J Am Coll Cardiol 2017;70:1-25. [Crossref] [PubMed]
- Mensah GA, Roth GA, Sampson UK, et al. Mortality from cardiovascular diseases in sub-Saharan Africa, 1990–2013: a systematic analysis of data from the Global Burden of Disease Study 2013: cardiovascular topic. Cardiovasc J Afr 2015;26:S6-10. [Crossref] [PubMed]
- Whitworth JAWorld Health Organization/International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/Internationa Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003;21:1983-92. [Crossref] [PubMed]
- WHO. Cardiovascular Disease: World Heart Day 2017. World Heal Organ. 2017;2017-8.
- Ogeng’o JA, Gatonga P, Olabu BO. Cardiovascular causes of death in an east African country: An autopsy study. Cardiol J 2011;18:67-72. [PubMed]
- Amegah AK. Tackling the Growing Burden of Cardiovascular Diseases in Sub-Saharan Africa. Circulation 2018;138:2449-51. [Crossref] [PubMed]
- Raphael DM, Roos L, Myovela V, et al. Heart diseases and echocardiography in rural Tanzania: Occurrence, characteristics, and etiologies of underappreciated cardiac pathologies. PLoS One 2018;13:e0208931. [Crossref] [PubMed]
- Mayige M, Kagaruki G. Tanzania Steps Survey Report. Ministry of Health and Social Welfare, and National Institute for Medical Research (NIMR) in Collaboration With World Health Organiztion, 2013. Available online: https://www.who.int/ncds/surveillance/steps/UR_ Tanzania_2012_STEPS_Report.pdf
- Global Status Report on Noncommunicable Diseases 2014: Attaining the Nine Global Noncommunicable Diseases Targets; A Shared Responsibility. World Heal Organization, 2014. Available online: https://reliefweb.int/ sites/reliefweb.int/files/resources/Global%20status%20 report%20on%20NCDs%202014-51b.pdf.
- WHO. Report on the status of major health risk factors for noncommunicable diseases: WHO African Region, 2015. WHO African Region. 2016:1-75.
- World Health Organization (WHO). (2014b). Non-communicable diseases Country Profiles 2014. World Health Organisation. pp. 120.
- Ministry of Health, Community Development, Gender, Elderly and Children. Strategic and Action Plan for the Prevention and Control of Non Communicable Diseases in Tanzania 2016 – 2020. 2016:1-144. Available online: https://www.worlddiabetesfoundation.org/sites/default/files/NCD%20Stategic%20Plan%202016%20-%202020.pdf
- Ngaleisoni F, Ruhago G, Mayige M, et al. Cost-effectiveness analysis of population-based tobacco control strategies in the prevention of cardiovascular diseases in Tanzania. PLoS One 2017;12:e0182113. [Crossref] [PubMed]
- WHO. Global status report on alcohol and health 2014ed. 2014:1-392.
- Mbatia J, Jenkins R, Singleton N. Prevalence of Alcohol Consumption and Hazardous Drinking, Tobacco and Drug Use in Urban Tanzania, and Their Associated Risk Factors. Int J Environ Res Public Health 2009;6:1991-2006. [Crossref] [PubMed]
- Muhamedhussein MS, Nagri ZI, Manji KP. Prevalence, Risk Factors, Awareness, and Treatment and Control of Hypertension in Mafia Island, Tanzania. Int J Hypertens 2016;2016:1281384. [Crossref] [PubMed]
- Stanifer JW, Cleland CR, Makuka GJ, et al. Prevalence, risk factors, and complications of diabetes in the Kilimanjaro region: A population-based study from Tanzania. PLoS One 2016;11:e0164428. [Crossref] [PubMed]
- Srinath Reddy K, Katan MB. Diet, nutrition and the prevention of hypertension and cardiovascular diseases. Public Health Nutrition 2004;7:167-86. [Crossref] [PubMed]
- Bovet P, Ross AG, Gervasoni JP, et al. Distribution of blood pressure, body mass index and smoking habits in the urban population of Dar es Salaam, Tanzania, and associations with socioeconomic status. Int J Epidemiol 2002;31:240-7. [Crossref] [PubMed]
- Kakarmath SS, Zack RM, Leyna GH, et al. Dietary determinants of serum total cholesterol among middle-aged and older adults: a population-based cross- sectional study in Dar es Salaam, Tanzania. BMJ Open 2017;7:e015028. [Crossref] [PubMed]
- Njelekela M, Sato T, Nara Y, et al. Nutritional variation and cardiovascular risk factors in Tanzania-rural-urban difference. S Afr Med J 2003;93:295-9. [PubMed]
- Mandha J, Buza J, Kassimu N, et al. Prevalence of Hypertension and Associated Risk Factors among Maasai Communities in Simanjiro, Tanzania. ACRI 2015;2:96-108. [Crossref]
- World Cancer Research Fund and The NCD Alliance. The link between food, nutrition, diet and non-communicable diseases. 2014;4. Available online: https://www.wcrf.org/sites/default/files/PPA_NCD_Alliance_Nutrition.pdf
- WHO. Global status report on noncommunicable diseases. World Heal Organ (WHO; Geneva). 2011.
- WHO. Global status report on non-communicable diseases 2014. World Health Organization, 2014;176.
- Kavishe B, Biraro S, Baisley K, et al. High prevalence of hypertension and of risk factors for non-communicable diseases (NCDs): A population based cross-sectional survey of NCDS and HIV infection in Northwestern Tanzania and Southern Uganda. BMC Med 2015;13:126. [Crossref] [PubMed]
- Dickie K, Micklesfield L, Chantler S, et al. Meeting physical activity guidelines is associated with reduced risk for cardiovascular disease in black South African women; a 5.5-year follow-up study. BMC Public Health 2014;14:498. [Crossref] [PubMed]
- WHO. Global Atlas on Cardiovascular Disease Prevention and Control. World Health Organization.2011. pp. 1-14.
- Unwin N, James P, Mclarty D, et al. Rural to urban migration and changes in cardiovascular risk factors in Tanzania: a prospective cohort study. BMC Public Health 2010;10:272. [Crossref] [PubMed]
- Mayige M, Kagaruki G, Ramaiya K, et al. Non communicable diseases in Tanzania: a call for urgent action. Tanzan J Health Res 2011;13:378-86. [PubMed]
- WHO. World Health Organization report on the global tobacco epidemic. Monitoring tobacco use and prevention policies. World Health Organization. 2017. pp. 1-263.
- WHO. World Health Organization report on the global tobacco epidemic, 2017; Country profile United Republic of Tanzania. World Health Organization. 2017. Available online: https://doi.org/
10.1787/9789264177949-147-en . - Ministry of Health (MoH) [Zanzibar]. Tanzania 2015-16 Demographic Health Survey and Malaria Indicator Survey. Tanzania 2015-16 Demogr Heal Surv Malar Indic Surv. 2015.
- Kapito-Tembo A, Muula AS, Rudatsikira E, et al. Smoking among in-school adolescents in Dar es Salaam, Tanzania: results from the Global Youth Tobacco Survey. Tanzan J Health Res 2011;13: [Crossref]
- Kidane A, Hepelwa A, Ngeh TE, et al. Healthcare Cost of Smoking Induced Cardiovascular Disease in Tanzania. J Health Sci (El Monte) 2015;3:117-22. [PubMed]
- Kapito-tembo A. Tanzania Demographic and Health Survey 2016. National Bureau of Statistics Dar Es Salaam, Tanzania Macro Calverton, Maryland, USA. 2016. pp. 1-482.
- WHO. Implementation of the WHO Framework Concention on Tobacco control in Tanzania 2007-2012.World Health Organization. 2012.
- World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization, 2009. Available online: https://apps.who.int/iris/handle/10665/44203
- WHO. A global brief on Hypertension: World Health Day 2013. World Heal Organ 2013:1-40.
- Peck RN, Green E, Mtabaji J, et al. Hypertension related diseases as a common cause of Hospital Mortality in Tanzania: a 3-Year prospective study. J Hypertens 2013;31:1806-11. [Crossref] [PubMed]
- Njelekela MA, Mpembeni R, Muhihi A, et al. Gender-related differences in the prevalence of cardiovascular disease risk factors and their correlates in urban Tanzania. BMC Cardiovasc Disord 2009;9:30. [Crossref] [PubMed]
- Isangula KG, Meda RJ. The Burden of Hypertension in the Rural and Urban populations of Tanzania: A review of Trends, Impacts and Response The Burden of Hypertension in the Rural and Urban populations of Tanzania: A Review of Trends, Impacts and Response. Tanzania. J Heal Sci 2018;1:41-52.
- Njelekela M, Negishi H, Nara Y, et al. Cardiovascular risk factors in Tanzania: a revisit. Acta Trop 2001;79:231-9. [Crossref] [PubMed]
- Edwards R, Unwin N, Mugusi F, et al. Hypertension prevalence and care in an urban and rural area of Tanzania. J Hypertens 2000;18:145-52. [Crossref] [PubMed]
- Makubi A, Hage C, Lwakatare J, et al. Contemporary aetiology, clinical characteristics and prognosis of adults with heart failure observed in a tertiary hospital in Tanzania: The prospective Tanzania Heart Failure (TaHeF) study. Heart 2014;100:1235-41. [Crossref] [PubMed]
- Zack RM, Irema K, Kazonda P, et al. Determinants of High Blood Pressure and Barriers to Diagnosis and Treatment in Dar es Salaam, Tanzania. J Hypertens 2016;34:2353-64. [Crossref] [PubMed]
- Galson SW, Staton CA, Karia F, et al. Epidemiology of hypertension in Northern Tanzania: a community-based mixed-methods study. BMJ Open 2017;7:e018829. [Crossref] [PubMed]
- Mosha NR, Mahande M, Juma A, et al. Prevalence, awareness and factors associated with hypertension in North West Tanzania. Glob Health Action. 2017;10:1321279. [Crossref] [PubMed]
- Swai AB, Mclarty D, Kitange H, et al. Low prevalence of risk factors for coronary heart disease in rural Tanzania. Int J Epidemiol 1993;22:651-9. [Crossref] [PubMed]
- Njelekela MA, Mpembeni R, Muhihi A, et al. Gender-related differences in the prevalence of cardiovascular disease risk factors and their correlates in urban Tanzania. BMC Cardiovasc Disord 2009;9:30. [Crossref] [PubMed]
- Zhou M, Astell-Burt T, Bi Y, et al. Geographical Variation in Diabetes Prevalence and Detection in China: Multilevel Spatial Analysis of 98,058 Adults. Diabetes Care 2015;38:72-81. [Crossref] [PubMed]
- International Diabetes Federation. IDF Diabetes Atlas. Vol. 8, International Diabetes Federation. 2017. 150 p.
- Aspray TJ, Mugusi F, Rashid S, et al. Rural and urban differences in diabetes prevalence in Tanzania: the role of obesity, physical inactivity and urban living. Trans R Soc Trop Med Hyg 2000;94:637-44. [Crossref] [PubMed]
- Mwangome M, Geubbels E, Klatser P, et al. Perceptions on diabetes care provision among health providers in rural Tanzania: A qualitative study. Health Policy Plan 2017;32:418-29. [PubMed]
- Muhamedhussein M, Manji KP, Sciences A. Prevalence, risk factors and awareness of hyperglycaemia in Mafia Island, Tanzania. African J Diabetes Med 2016;9:1-4.
- Cleland CR, Burton MJ, Hall C, et al. Diabetic retinopathy in Tanzania: prevalence and risk factors at entry into a regional screening programme. Trop Med Int Health 2016;21:417-26. [Crossref] [PubMed]
- Chiwanga FS, Njelekela MA. Diabetic foot: prevalence, knowledge, and foot self-care practices among diabetic patients in Dar es Salaam, Tanzania – a cross-sectional study. J Foot Ankle Res 2015;8:20. [Crossref] [PubMed]
- Shayo GA, Mugusi FM. Prevalence of obesity and associated risk factors among adults in Kinondoni municipal district, Dar es Salaam Tanzania. BMC Public Health 2011;11:365. [Crossref] [PubMed]
- Pangani IN, Kiplamai FK, Kamau JW, et al. Prevalence of Overweight and Obesity among Primary School Children Aged 8–13 Years in Dar es Salaam City, Tanzania. Adv Prev Med 2016;2016:1345017. [Crossref] [PubMed]
- Ajayi IO, Adebamowo C, Adami HO, et al. Urban–rural and geographic differences in overweight and obesity in four sub-Saharan African adult populations: a multi-country cross-sectional study. BMC Public Health 2016;16:1126. [Crossref] [PubMed]
- Muhihi AJ, Njelekela MA, Mpembeni R, et al. Obesity, Overweight, and Perceptions about Body Weight among Middle-Aged Adults in Dar es Salaam, Tanzania. ISRN Obes 2012;2012:368520. [Crossref] [PubMed]
- Mpembeni RN, Muhihi AJ, Maghembe M, et al. Overweight, Obesity and perceptions about body weight among primary schoolchildren in dar es salaam, Tanzania. Tanzan J Health Res 2014;16:304-11. [Crossref] [PubMed]
- Mayige M. Prevention of non-communicable diseases in Tanznaia using an intersectoral approach. Tech Rep 2016. doi:
10.13140/RG.2.1.3976.1047 . - Ngalesoni FN, Ruhago GM, Mori AT, et al. Cost-effectiveness of medical primary prevention strategies to reduce absolute risk of cardiovascular disease in Tanzania: a Markov modelling study. BMC Health Serv Res 2016;16:185. [Crossref] [PubMed]
- WHO. A Comprehensive Global Monitoring Framework Including Indicators and a Set of Voluntary Global Targets For The Prevention and Control of Noncommunicabale World Health Organization. 2012:1-23. Available online: https://www.who.int/nmh/events/2012/discussion_paper2_20120322.pdf
Cite this article as: Roman WP, Martin HD, Sauli E. Cardiovascular diseases in Tanzania: The burden of modifiable and intermediate risk factors. J Xiangya Med 2019;4:33.