Prevalence of hypertension and associated risk factors among a group of prisoners in Yaoundé Central Prison: a cross-sectional study
Introduction
Hypertension is a major public health problem in the world, with a global prevalence estimated at 1.13 billion in 2015 and responsible for about 18 million people deaths yearly (1,2). Otherwise, more than 50% of deaths from coronary heart disease (CHD) and stroke occurred in people with hypertension (3). By 2025, it is estimated that about 1.5 billion of the world’s population will be hypertensive. The prevalence in the United States of America (USA) was estimated at 30.2% in 2015 (4). With American College of Cardiology (ACC) and American Heart Association (AHA) new guidelines recommendations for diagnosis of elevated blood pressure and therapy, the burden is increasing to 46% of the population in USA (5).
Racial disparities in hypertension prevalence and control are recognized for the past 4 decades (6,7). In Africa, hypertension remains one of the principal cardiovascular risk factors affecting approximately 30% of adults (8). Recent studies on hypertension in Nigeria and in the Democratic Republic of Congo showed similar results with respectively 28.9% and 30.9% of prevalence (9,10). In Cameroon, the prevalence is increasing in the general population, rising from 20.8% in 2007 to 24.2% in 2012 and 29.7% in 2015 ame (11-13). There is a regional disparity between rural and urban area, with a rural prevalence of hypertension lower than the urban one but rising with time (14-16).
Blood pressure has been shown to vary according to constitutional factors such as age, weight, race and sex. The association between these factors and hypertension is known, although the mechanisms involved remain obscure. Other factors are also described: heredity, genetic predisposition, the influence of the environment, lifestyles such as salt consumption and sedentary lifestyle. However, the contribution of other factors such as stress (professional, family and social) is far from unanimous (17). The westernization of lifestyle, as well as the lack of information of patients on their pathology resulting in the refusal of treatment for life in the absence of obvious symptoms and the impact of traditional medicine in rural areas, surely explain the prevalence of elevated blood pressure in our environment. The resulting morbidity and mortality are all the more important (18).
Several studies in western countries showed an increased prevalence of hypertension among prisoners (19-21). Overpopulation, poor nutrition and lack of preventive strategies are incriminated in this prevalence. In Cameroon, a previous study in 1992 reported psychological pressure, promiscuity associated with increased prevalence of hypertension (22). With increase carceral population in Cameroon, it was therefore important for us to assess the prevalence of hypertension among prisoners to identify the associated factors (23).
Methods
Ethical statement
This work was approved by the institutional board of the Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon. This work was carried out in accordance with the declaration of Helsinki (24).
Study design and setting
We conducted a cross-sectional study from January to July 2017 among prisoners at the Yaoundé Central Prison. This is the main prison in Yaoundé, the capital city of Cameroon (SSA), with a population of 2 million individuals. The carceral population is evaluated at 4,859 inmates in July 2017. This prison was initially built for 800 prisoners. It consists of 206 rooms divided into 13 quarters. Promiscuity and malnutrition rate are high among prisoners. Bedding condition are poor: most of prisoners sleep on mattress laid on the floor. Physical activities are rare (25). There are only two doctors for managing all prisoners.
Variables and measurements
We included consenting subjects, seen in the in-prison clinic. Subjects were approached regardless of the duration of diagnosis or follow-up. Pregnant women, patients with in-prison stay less than three months, patients not seen at the second passage and non-consenting patients were excluded. According hypertension prevalence in Cameroon, minimal sampling was calculated at 320 prisoners. Administrative authorizations were obtained prior to the completion of this study.
The screening was conducted by trained medical personnel at the clinic. All participants were subjected to a face-to-face interview. All prisoners, consenting to participate, where seen twice at 1-month interval. Data were collected (using a standardized questionnaire) on demographics, incarceration characteristics (duration, the reason of detention, the severity of condemnation, the number of monthly visit), smoking habits and alcohol consumption, diabetes and hypertension history including drugs treatment and complications and other cardiovascular risk factors.
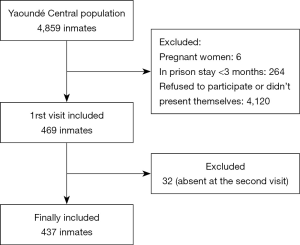
The physical examination included BP and anthropometric measurements. BP (systolic and diastolic) was measured in chair-seated patients at left arm after 5 minutes by the same medical personnel. BP measurements were performed using automated sphygmomanometers (OMRON, Kyoto, Japan), with appropriate cuff size. Mean BP of both visits was registered. Weight (in kg) was measured in participants on light clothing using an automated scale. Height (in m) was measured using a wooden platform and a height rule. Body mass index was calculated as weight (kg)/height (m) × height (m). Waist circumference was measured between the iliac crest and the lower rib margin and the hip circumference was measured at the intertrochanteric level. The selection process is summarized on Figure 1.
Definitions
Hypertension was defined as a BP ≥140 mmHg (systolic) and/or 90 mmHg (diastolic). People with a previous diagnosis or treatment for hypertension were also considered as hypertensive. Obesity was defined as a BMI of ≥30 kg/m2, and overweight was defined as a BMI between 25 and 29.9. Sedentary lifestyle was defined as the absence of any physical activity (absence of at least 3 walking episodes of 45 min in a week).
Waist circumference >94 cm in men or 80 cm in women was considered to be high. Excessive alcohol consumption was based on intake either more than 3 (2 for women) standard glasses of wine per day or more than 10 (5 for women) local beers per week. Traditional alcohol beverage was not assessed. Participants who smoked at least one cigarette per day were classified as current smokers.
Low social class was determined by monthly income less than 86.3 $US, middle social class by income between 86.3 and 258.9 $US and high social class by income above this amount.
Reason for detention was classified according Cameroon’s penal code (2016 version) into felonies or crimes (an infraction punishable with death or with loss of liberty for a maximum of more than 10 years and fine where the law so provides) and offense (an infraction punishable with loss of liberty or with fine, where the loss of liberty may be for more than 10 days but not for more than 10 years, and the fine more than 43.2 $US). The crimes may be subdivided into minor (use or selling of drugs, the unauthorized use of a weapon, or robbery) and major (homicide, rape or embezzlement of public funds) crimes (26).
The monthly visit was classified as inexistent (if no visit), low (≤2 visits), frequent (3–19 visits), and very frequent (≥10 visits).
Weekly leave permission of 0 was considered as low. A rate of 1–2 leaves per week was classified as average as and more than 2 per week as high.
Promiscuity was defined by a cell occupation rate of 5–19 inmates per cell. High promiscuity by a number of 20–40 inmates per cell and very high promiscuity by >40 inmates per cell. A number <5 inmates by cell defined no promiscuity.
Sentence severity was classified into short (<5 years), average (5 to less than 15 years) and severe (>15 years). By the same, an incarceration length <5 years was considered as short, between 5 and 15 years as average and more than 15 years was high.
Statistical analysis
Data were analyzed using Statistical Package for Social Sciences (SSPS Inc., Chicago, Illinois, USA) V.20.0 and EPI-INFO V.3.5 software. Results are summarized as counts and percentages for qualitative variables and mean and standard deviations (SD) for quantitative variables. Groups comparisons used Chi-square tests and equivalents for qualitative variables and student t-test, analysis of variance for quantitative variables We calculated the odds for each parameter studied in inmates having hypertension compared with those who do not have hypertension. A P value <0.05 was used to characterize statistically significant results. Using significant parameters, a multivariate analysis by logistic regression will be made.
Results
Participants
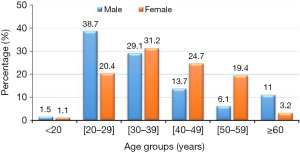
A total of 437 inmates were included, of which 344 (78.7%) were males, and the mean age was 37 years (95% CI: 35.9–38.3). The 20 to 39 years age group were the most frequent with 281 (64.7%) patients (Figure 2). The mean prison stay was 29.1 months (95% CI: 25.7–32.8). Among them, 173 (39.6%) inmates were hypertensive. Mean systolic BP was 128.4 mmHg (95% CI: 126.3–130.7). Mean diastolic BP was 84.4 mmHg (95% CI: 81.7–84.2). Both mean systolic and mean diastolic BP increased with age (P<0.001). Isolated diastolic hypertension was found in 39 (22.5%) of hypertensive inmates, while isolated systolic hypertension and systolic-diastolic hypertension where respectively found in 35 (20.2%) and 99 (57.3%) hypertensive inmates.
Main data
Sedentary lifestyle (91.1%), smoking (31.6%) and alcohol (28.1%) were the main cardiovascular risk factors among inmates. The CVRFs are presented in Table 1. Age ≥40 years (P<0.0001), alcohol consumption (P=0.04) and obesity (P<0.0001) were associated with hypertension.
Table 1
| Variables | Overall | Hypertension+, n (%) | Hypertension−, n (%) | OR (95% CI) | P |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 341 | 136 (78.6) | 205 (77.7) | 1.0 (0.7–1.7) | 0.4 |
| Female | 96 | 37 (21.4) | 59 (22.3) | ||
| Age ≥40 years | 150 | 89 (59.3) | 51 (40.7) | 3.5 (2.3–5.3) | <0.0001 |
| Social class | |||||
| Low | 241 | 94 (39.0) | 147 (61.0) | 0.9 (0.6–1.4) | 0.39 |
| Middle | 74 | 18 (24.3) | 56 (75.7) | 0.4 (0.2–0.8) | 0.001 |
| High | 122 | 61 (50.0) | 61 (50.0) | 1.9 (1.2–2.8) | 0.002 |
| Diabetes | 27 | 13 (48.1) | 14 (51.9) | 1.4 (0.7–3.2) | 0.2 |
| Obesity | 51 | 27 (52.9) | 24 (47.1) | 1.8 (1–3.3) | 0.02 |
| Smoking | 138 | 62 (44.9) | 76 (55.1) | 1.4 (0.9–2.1) | 0.06 |
| Alcohol consumption | 123 | 57 (46.3) | 66 (53.7) | 1.5 (0.9–2.2) | 0.04 |
| Sedentary lifestyle | 398 | 158 (39.7) | 240 (60.3) | 1.0 (0.5–2.1) | 0.44 |
| Visit rate (per month) | |||||
| Inexistent | 54 | 20 (37.0) | 34 (63.0) | 0.9 (0.5–1.6) | 0.34 |
| Low | 197 | 83 (41.9) | 114 (58.1) | 1.2 (0.8–1.8) | 0.18 |
| Frequent | 143 | 52 (36.4) | 91 (63.6) | 0.8 (0.5–1.2) | 0.16 |
| Very frequent | 43 | 18 (41.9) | 25 (58.1) | 1.11 (0.6–2.1) | 0.69 |
| Weekly permission leave | |||||
| Low | 412 | 164 (39.8) | 248 (60.2) | 1.2 (0.5–2.7) | 0.36 |
| Average | 17 | 8 (47.1) | 9 (52.9) | 1.4 (0.5–3.6) | 0.26 |
| High | 8 | 2 (25.0) | 6 (75.0) | 0.5 (0.05–4.9) | 0.3 |
| Judiciary sentence | |||||
| Accused guilty | 226 | 81 (35.8) | 145 (64.2) | 0.7 (0.5- 1.0) | 0.04 |
| Short sentence | 94 | 36 (38.3) | 58 (61.7) | 0.9 (0.6–1.5) | 0.38 |
| Average sentence | 74 | 28 (37.8) | 46 (62.2) | 0.9 (0.5–1.5) | 0.37 |
| Long sentence | 43 | 28 (65.1) | 15 (34.9) | 3.2 (1.7–6.2) | 0.0002 |
| Reason of detention | |||||
| Offense | 250 | 86 (34.4) | 164 (65.6) | 0.6 (0.4–0.9) | 0.005 |
| Minor crimes | 67 | 22 (32.8) | 45 (67.2) | 0.7 (0.4–1.2) | 0.09 |
| Major crimes | 120 | 66 (55.0) | 54 (45.0) | 2.4 (1.6–3.8) | <0.0001 |
| Length of incarceration | |||||
| Low | 387 | 141 (36.4) | 246 (63.6) | 0.3 (0.2–0.6) | <0.0001 |
| Average | 41 | 25 (61.0) | 16 (39.0) | 2.6 (1.3–5.0) | 0.002 |
| Long | 9 | 7 (77.8) | 2 (22.2) | 5.5 (1.1–26.9) | 0.02 |
| Promiscuity | |||||
| No promiscuity | 52 | 29 (55.8) | 23 (44.2) | 2.2 (1.2–3.8) | 0.006 |
| Low promiscuity | 89 | 37 (41.6) | 52 (58.4) | 1.1 (0.7–1.8) | 0.32 |
| High promiscuity | 106 | 42 (39.6) | 64 (60.4) | 1.0 (0.6–1.6) | 0.49 |
| Very high promiscuity | 190 | 65 (34.2) | 125 (65.8) | 0.7 (0.4–1) | 0.03 |
Low social class was the most frequent, found in 241 inmates (55.1%), followed by a high social class in 122 inmates (27.9%). Among those inmates, 226 (51.7%) of them were accused guilty, 94 (21.5%) were condemned for less than 5 years, 74 (16.9%) were condemned for 5 to 15 years and 43 (9.8%) for more than 15 years. Visit rate was inexistent in 54 (12.4%), low in 198 (45.3%), frequent in 143 (32.7%) and very frequent in 43 (9.8%) inmates. Weekly permission leave was low for 412 (94.3%), average for 17 (3.9%), and high for 8 (1.8%) inmates. Promiscuity was common in prison cells. According to cell occupation rate, very high promiscuity was frequent in 190 (43.5%), followed by high promiscuity in 106 (24.2%), promiscuity in 89 (20.4%) and no promiscuity in 52 (11.9%) inmates.
Many inmates exhibit comorbidities. Tuberculosis was the main comorbidity in 37 (8.5%) inmates, followed by HIV in 25 (5.7%) inmates and scabies in 21 (4.8%) inmates.
Many detention variables were associated with hypertension in univariate analysis. Social class (preferentially in a higher class (P=0.002) and middle social class (P=0.001). There was no association with low social class (P=0.39). Concerning reason of detention, offense (P=0.005) and major crime (P<0.0001) were associated with hypertension. The judiciary sentence been accused of guilty (P=0.049) and also having a severe sentence (P=0.0002) were associated with hypertension. The incarceration length was also associated with hypertension with P<0.0001 for short stay, P=0.002 for average stay and P=0.02 for a long stay. Cell occupation rate was also associated with hypertension, with P=0.03 in very high promiscuity cells inhabitants and P=0.006 for no promiscuity cells inhabitants. There was no association with a monthly visit and weekly leave authorization.
In multivariate analysis, only age (>40 years), middle social class and alcohol consumption were associated with hypertension among inmates (Table 2).
Table 2
| Risk factor | OR (95% CI) | P |
|---|---|---|
| No promiscuity | 1.8 (0.9–3.8) | 0.12 |
| Very high promiscuity | 0.8 (0.5–1.4) | 0.59 |
| Long sentence | 1.6 (0.7–3.6) | 0.22 |
| Offenses | 1.2 (0.6–2.3) | 0.71 |
| Major crimes | 1.4 (0.8–2.4) | 0.24 |
| Average length of incarceration | 1.8 (0.8–4) | 0.13 |
| Long length of incarceration | 3 (0.5–16.9) | 0.21 |
| Middle social class | 0.5 (0.2–0.9) | 0.02 |
| High social class | 1.2 (0.7–2) | 0.47 |
| Age ≥40 years | 3.3 (2–5.2) | <0.0001 |
| Obesity | 1 (0.5–2.1) | 0.87 |
| Alcohol consumption | 1.7 (1–2.7) | 0.02 |
Discussion
We carried out this cross-sectional study to assess the prevalence of hypertension and their associated risk factors among a group of prisoners in an sub-Saharan African setting. This study represents the first published analysis of hypertension in a specific population of inmates in Africa.
Non-communicable disease among prisoners has not been fully explored in Africa (27-29). Hypertension’s burden among prisoners particularly is still poorly known in Africa. Few studies on its prevalence and risk factors have been carried out (22). Hypertension prevalence is known to be increased among inmates in a western country (30-32). However, there is no data in Africa and particularly in Cameroon for its prevalence and risk factors.
This study should be interpreted in light of some limitations. Our study population was small compared to other studies done on this subject. Another limitation was the fact that the study relied on a population census that was not designed to explicitly measure the effect of exposure to incarceration (length). Our capacity to make causal inferences is limited by the cross-sectional design of the study.
Hypertension prevalence was 39.6% in Yaoundé central prison. This is higher than 21.4% found by Ndongmo et al. in 1992 (22). But hypertension definition and classification were different in those days resulting in a probable misdiagnosis (33). This hypertension prevalence was also higher than the national hypertension prevalence, similarly to Wang et al. findings (30). Main CVRFs were a sedentary lifestyle, smoking, alcohol, and obesity. As reported by Herbert and Ritter, physical activity and obesity were low among prisoners, while smoking and alcohol consumption are increased (34,35). Increased hypertension prevalence could be related to stress and poor feeding of prisoners (36,37). As in the normal population, hypertension prevalence increased with age.
Detention variables associated with hypertension included:
- Social class: preferentially in a higher class (P=0.002) and middle social class (P=0.001). It might due to the reduction of income or increased stress;
- Length of incarceration: short (P<0.0001), average (P=0.002) and long incarceration (P=0.02) were associated with hypertension. This was similar to Silverman et al. findings, showing an increase of hypertension with incarceration duration (31). Otherwise, Howell et al. showed that BP is high or uncontrolled among ancient prisoners (32);
- The reasons for detention: major offense (P=0.04) and major crime (P<0.0001) were associated with hypertension. This can be related to sentence severity;
- Judiciary sentence: been accused guilty (P=0.049) and also having a severe sentence (P=0.0002) were associated with hypertension. This could be related to the incarceration duration. People accused guilty can spend years in prison before any trial;
- Cell occupation rate: very high promiscuity cells inhabitants (P=0.03) and no promiscuity cells inhabitant (P=0.006) were also associated with hypertension. We hypothesized that no promiscuity cell inhabitants were from high social class and people living in very high promiscuity stress are more at risk of stress.
Regarding the high prevalence of hypertension and some CVRFs among prisoners, there is a need to implement preventive strategies for hypertension. This goes through a precise screening of patients with multiples CVRFs, diet modification, alcohol and smoking cessation policies and increase physical activity. It would be therefore important to increase caregiver’s number in order to optimize prisoners care. Meda et al. emphasized on health promotion among prisoners for preventing diseases and strengthening prisoners’ resilience but they only prioritized infectious diseases (38).
Conclusions
This study is the first of its type in Cameroon. Prevalence of hypertension in the Yaoundé Central Prison of was 39.6%. Risk factors for hypertension among prisoners included detention variables such as middle and high social class inmates, the sentence for a major crime or major offense, a severe sentence, the incarceration length, and no and high promiscuity. Due to the high prevalence of hypertension among those group of prisoners, there is a need to implement preventive strategies for hypertension in prison.
Acknowledgments
We thank all the stall of the infirmary of the Yaoundé Central Prison and its director. We would like also to thank Professor Marc Leeman for his valuable contribution to improve the quality of English and the scientific value of this research.
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.05.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). This work was approved by the institutional board of the Faculty of Medicine and Biomedical Sciences, University of Yaoundé I, Cameroon and written informed consent was obtained from all patients.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 2018;39:3021-104. [Crossref] [PubMed]
- NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in blood pressure from 1975 to 2015: a pooled analysis of 1479 population-based measurement studies with 19•1 million participants. Lancet 2017;389:37-55. [Crossref] [PubMed]
- Ford ES. Trends in mortality from all causes and cardiovascular disease among hypertensive and non-hypertensive adults in the United States. Circulation 2011;123:1737-44. [Crossref] [PubMed]
- Whitworth JAWorld Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003;21:1983-92. [Crossref] [PubMed]
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. J Am Soc Hypertens 2018;12:579.e1-e73. [Crossref] [PubMed]
- Cruickshank JK, Beevers DG. Epidemiology of Hypertension: Blood Pressure in Blacks and Whites. Clin Sci 1982;62:1-6. [Crossref] [PubMed]
- Lackland DT. Racial Differences in Hypertension: Implications for High Blood Pressure Management. Am J Med Sci 2014;348:135-8. [Crossref] [PubMed]
- World Health Organization. GLOBAL STATUS REPORT on non-communicable diseases 2014. WorldHealth Organisation, 2014:66-77. Available online: https://www.who.int/nmh/publications/ncd-status-report-2014/en/
- Adeloye D, Basquill C, Aderemi AV, et al. An estimate of the prevalence of hypertension in Nigeria: a systematic review and meta-analysis. J Hypertens 2015;33:230-42. [Crossref] [PubMed]
- Bayauli PM, M’Buyamba-Kayamba JR Jr, Lemogoum D, et al. Cardiovascular risk factors among the inhabitants of an urban Congolese community: results of the VITARAA Study. IJC Metab Endocr 2014;4:33-8. [Crossref]
- Kengne AP, Awah PK, Fezeu L, et al. The burden of high blood pressure and related risk factors in urban sub-Saharan Africa: evidences from Douala in Cameroon. Afr Health Sci 2007;7:38-44. [PubMed]
- Kengne AP, Ntyintyane LM, Mayosi BM. A systematic overview of prospective cohort studies of cardiovascular disease in sub-Saharan Africa. Cardiovasc J Afr 2012;23:103-12. [Crossref] [PubMed]
- Kingue S, Ngoe CN, Menanga AP, et al. Prevalence and Risk Factors of Hypertension in Urban Areas of Cameroon: A Nationwide Population-Based Cross-Sectional Study. J Clin Hypertens (Greenwich) 2015;17:819-24. [Crossref] [PubMed]
- Mbanya JC, Minkoulou EM, Salah JN, et al. The prevalence of hypertension in rural and urban Cameroon. Int J Epidemiol 1998;27:181-5. [Crossref] [PubMed]
- Arrey WT, Dimala CA, Atashili J, et al. Hypertension, an Emerging Problem in Rural Cameroon: Prevalence, Risk Factors, and Control. Int J Hypertens 2016;2016:5639146. [Crossref] [PubMed]
- Lemogoum D, Van de Borne P, Lele CEB, et al. Prevalence, awareness, treatment, and control of hypertension among rural and urban dwellers of the Far North Region of Cameroon. J Hypertens 2018;36:159-68. [Crossref] [PubMed]
- Beevers G, Lip GY, O’Brien E. ABC of hypertension: The pathophysiology of hypertension. BMJ 2001;322:912-6. [Crossref] [PubMed]
- van de Vijver S, Akinyi H, Oti S, et al. Status report on hypertension in Africa--consultative review for the 6th Session of the African Union Conference of Ministers of Health on NCD’s. Pan Afr Med J 2013;16:38. [PubMed]
- Wilper AP, Woolhandler S, Boyd JW, et al. The Health and Health Care of US Prisoners: Results of a Nationwide Survey. Am J Public Health 2009;99:666-72. [Crossref] [PubMed]
- Maruschak L, Berzofsky M, Unangst J. Medical Problems of State and Federal Prisoners and Jail Inmates, 2011-12. Available online: https://www.bjs.gov/content/pub/pdf/mpsfpji1112.pdf
- Maruschak L, Chari KA, Simon AE, et al. National Survey of Prison Health Care: Selected Findings. Natl Health Stat Report 2016;1-23. [PubMed]
- Ndongmo R. Profil Psychologique et facteurs de risque cardiovasculaire chez un groupe de prisonniers de Yaoundé. Yaoundé: Faculté de Médecine et des Sciences Biomédicales, 1992.
- Cameroon | World Prison Brief. Available online: http://www.prisonstudies.org/country/cameroon
- Association Médicale Mondiale. Déclaration d’Helsinki de l’Association Médicale Mondiale: principes éthiques applicables aux recherches médicales sur des sujets humains. Available online: https://www.wma.net/fr/policies-post/declaration-dhelsinki-de-lamm-principes-ethiques-applicables-a-la-recherche-medicale-impliquant-des-etres-humains/
- Special Rapporteur on Prisons and Conditions of detention in Africa. Prisons in Cameroon. Report of the Special Rapporteur on Prisons and Conditions of detention in Africa. The African Commission on Human And Peoples’ Rights.
- Cameroon’s penal code. Sect 21, 2016/007. Available online: https://www.wipo.int/edocs/lexdocs/laws/en/cm/cm014en.pdf
- Telisinghe L, Charalambous S, Topp SM, et al. HIV and tuberculosis in prisons in sub-Saharan Africa. Lancet 2016;388:1215-27. [Crossref] [PubMed]
- Noeske J, Kuaban C, Amougou G, et al. Pulmonary tuberculosis in the Central Prison of Douala, Cameroon. East Afr Med J 2006;83:25-30. [Crossref] [PubMed]
- Noeske J, Ndi N, Mbondi S. Controlling tuberculosis in prisons against confinement conditions: a lost case? Experience from Cameroon. Int J Tuberc Lung Dis 2011;15:223-7. i. [PubMed]
- Wang EA, Redmond N, Dennison Himmelfarb CR, et al. Cardiovascular Disease in Incarcerated Populations. J Am Coll Cardiol 2017;69:2967-76. [Crossref] [PubMed]
- Silverman-Retana O, Lopez-Ridaura R, Servan-Mori E, et al. Cross-Sectional Association between Length of Incarceration and Selected Risk Factors for Non-Communicable Chronic Diseases in Two Male Prisons of Mexico City. PLoS One 2015;10:e0138063. [Crossref] [PubMed]
- Howell BA, Long JB, Edelman EJ, et al. Incarceration History and Uncontrolled Blood Pressure in a Multi-Site Cohort. J Gen Intern Med 2016;31:1496-502. [Crossref] [PubMed]
- Carey RM. The 1984 Report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med 1984;144:1045-57. [Crossref] [PubMed]
- Herbert K, Plugge E, Foster C, et al. Prevalence of risk factors for non-communicable diseases in prison populations worldwide: a systematic review. Lancet 2012;379:1975-82. [Crossref] [PubMed]
- Ritter C, Stöver H, Levy M, et al. Smoking in prisons: The need for effective and acceptable interventions. J Public Health Policy 2011;32:32-45. [Crossref] [PubMed]
- Massoglia M. Incarceration as Exposure: The Prison, Infectious Disease, and Other Stress-Related Illnesses. J Health Soc Behav 2008;49:56-71. [Crossref] [PubMed]
- Edwards JSA, Williams P, Hartwell HJ, et al. Comments on prison foodservice: England vs. Australia. J Foodserv 2009;20:153-6. [Crossref]
- Meda N, Traore K, Diendéré E, et al. Promotion de la santé des prisonniers au Burkina Faso: application de la deuxième version de la classification internationale des soins primaires (CISP-2) pour l’identification des besoins. Rev DÉpidémiologie Santé Publique 2013;61:S224. [Crossref]
Cite this article as: Tiodoung Timnou A, Boombhi J, Simeni Njonnou SR, Jingi AM, Nkem Efon K, Bâ H, Mfeukeu-Kuate L, Nganou-Ngnindjo CN, Ndongo Amougou S, Ntsama Essomba MJ, Kengni Kebiwo O, Talbit Ndjonya S, Poka Mayap V, Menanga AP, Kingue S. Prevalence of hypertension and associated risk factors among a group of prisoners in Yaoundé Central Prison: a cross-sectional study. J Xiangya Med 2019;4:22.