
The role of real time 3D-transesophageal echocardiography for safe and successful atrial septal defect closure
Introduction
Real-time three-dimensional transesophageal echocardiography (RT3D-TEE) has emerged as a revolutionary innovation in cardiovascular imaging that provides dramatically improved anatomic assessment of cardiac structures, such as atrial septal defects (ASDs) (1-3). Due to the complex and morphologically unpredictable 3D anatomy of the interatrial septum, en face viewing in 3D-TEE provides incremental value to ASD assessment and the surrounding fossa with a more accurate determination of ASD maximal diameter, overall size and shape compared to the limited sizing ability of 2D imaging. This benefit is even more appreciated in complex septal defects where balloon sizing may not be feasible or an appropriately sized septal occluder may not be available. Furthermore, 3D imaging offers the potential to clearly and comprehensively define the dynamic morphology of the defect, which has been shown to change during the cardiac cycle. A 360-degree evaluation is provided of the surrounding rim tissue that is needed to adequately anchor an ASD occluder device (4,5). 3D-TEE enhances pre-procedural planning and device selection as well as intra-procedural placement of the appropriate device for ASD closure (6). Intraoperatively, RT3D-TEE enhances the detection of the position of a catheter or a device relative to its surrounding cardiac environment and can provide clear images that can confirm appropriate seating of the right and left atrial discs, evidence for residual shunting, and the relationship to surrounding structures such as the aortic root and posterior atrial wall. This improved imaging fidelity improves both safety and efficacy of these procedures (4,6-8). The aim of this manuscript is to present a series of cases where 3D-TEE was used during percutaneous ASD closure to enhance pre- and intra-procedural decision making to facilitate a successful result.
Case presentations
Case 1
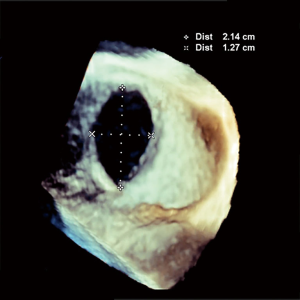
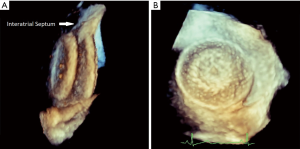
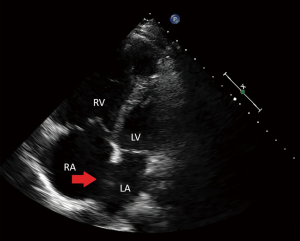
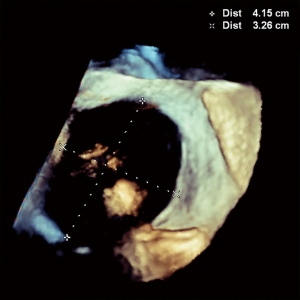
A 64-year-old female with no previous cardiac history progressively developed exertional pre-syncope and decreased endurance. Work-up revealed a dilated right ventricle and 3D-TEE illustrated a 21×13 mm secundum ASD (Figure 1). A 20 mm Amplatzer™ Septal Occluder (ASO) was selected for closure based on 3D-TEE sizing. During the procedure, RT3D-TEE aided in directly visualizing parallel apposition of the deployed left atrial ASO disk to the left atrial septum. After the right atrial disk was deployed, color Doppler imaging ensured appropriate device seal. Both left and right atrial disks were clearly identified with 3D right atrium and left atrium en face views confirming circumferential capture of the rim tissue (Figure 2). Adequate room posteriorly was ensured with 3D-TEE and helped show stability post-release with no evidence of encroachment into the aorta anteriorly.
Case 2
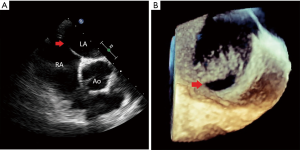
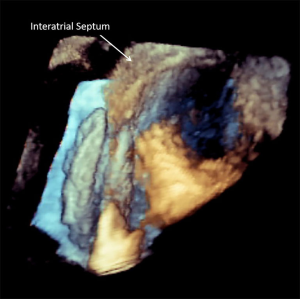
A 49-year-old female with a history of multiple strokes without evidence of atrial fibrillation or carotid disease presents for evaluation. 2D-TTE was suggestive of a patent foramen ovale (PFO), and she was referred for PFO closure with RT3D-TEE. Intra-procedure interrogation of the interatrial septum by 3D-TEE revealed a 9 mm secundum ASD with bidirectional shunting as opposed to a PFO (Figure 3). This information directly influenced device closure selection, and a 10 mm ASO device was selected. In a similar manner to patient #1, after correctly illustrating this patient’s atrial septal pathology, RT3D-TEE was used to ensure appropriateness of rim tissue to accommodate the ASO device. Post-deployment, 3D-TEE exhibited excellent device seal and purchase of all rim tissue without encroachment anteriorly in the aorta (Figure 4).
Case 3
A 35-year-old male without past medical history developed progressive chest pain and shortness of breath. Workup was negative for myocardial ischemia, but 2D-TTE showed significant right ventricular enlargement and moderate pulmonary hypertension. Also noted on 2D-TTE imaging was a secundum ASD with an estimated maximum diameter of 34 mm (Figure 5). The patient was then referred for percutaneous ASD closure. Pre-procedural 3D-TEE was performed and disclosed the true extent of this large atrial defect, measuring 42×33 mm (Figure 6). 3D images showed minimal rim tissue for device deployment and capture; 3D-TEE clearly revealed that this defect was not amenable to percutaneous closure. Therefore, the patient was referred to surgery and underwent a successful open surgical repair of the large secundum defect.
Discussion
RT3D-TEE has become an indispensable imaging technique for secundum ASD closure affording precise imaging of complex, dynamic structural heart defects and their associated interventions. Limitations that exist in the evaluation of 3D interatrial septal structures using 2D echocardiography are overcome through the unique views provided in 3D imaging. Furthermore, with an enhanced ability to detect the position of a catheter or a device relative to its surrounding cardiac environment, it offers the potential for shorter and safer interventional operations. Arguably, through facilitating procedural success, RT3D-TEE likely improves patient outcomes.
Two other case reports have discussed the benefits of 3D-TEE imaging in diagnosis and closure of a rare X-shaped secundum ASD and multiple atrial defects in a single patient (9,10). This is the first case series in literature to highlight the various advantages of RT3D-TEE in the closure of these unique secundum type ASD cases. Our three secundum type ASDs were evaluated through the employment of both 3D- and 2D-echocardiography. RT3D-TEE provides accurate assessment of the size and morphology of the defects for appropriate device selection and facilitation of the interventional procedure. For case #1, 3D-TEE ensured adequate sizing of the device and sufficient buffer room around the device to mitigate the risk of erosion. For case #2, 3D-TEE allowed the operators to realize that the defect was, in fact, a small secundum ASD, and not a PFO, as was suggested by the 2D images. This had a significant impact on device selection. In the last patient, 3D-TEE provided an accurate assessment of the true size of the defect which helped determine that open surgical closure was needed.
3D echocardiography is prone to the same types of artifacts that can be encountered in 2D echocardiography. However, when these artifacts are displayed in a 3D format, some can be difficult to distinguish compared to others are that unique to image acquisition and postprocessing. Variations in gain setting could overestimate orifice areas, while dropout artifacts could be misinterpreted as holes. To maximize accurate measurement of an ASD on 3D imaging, it is necessary to crop down the image to the plane where the orifice is the smallest. Stitching artifacts can reduce image quality making analysis more difficult and reverberations tend to increase the length of the catheter on image (11).
Conclusions
RT3D-TEE is becoming a more routinely established imaging technique for structural heart disease and offers a more comprehensive understanding of secundum type ASDs compared to 2D TTE. It significantly expands the diagnostic capabilities of cardiac ultrasound, allowing the visualization of cardiac anatomy, pathology, and devices in a 3D format easily appreciated by operators. RT3D-TEE should be an essential imaging tool for guiding and assessing ASD device closure. Improved accuracy of the initial diagnostic assessment and minimized complications during percutaneous closure will greatly impact the success and safety of ASD interventions and patient outcomes.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2019.03.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Carroll JD, Webb JG. editors. Structural heart disease interventions. Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins, 2012.
- Buccheri S, Costanzo L, Tamburino C, et al. Reference Values for Real Time Three-Dimensional Echocardiography-Derived Left Ventricular Volumes and Ejection Fraction: Review and Meta-Analysis of Currently Available Studies. Echocardiography 2015;32:1841-50. [Crossref] [PubMed]
- Charakida M, Pushparajah K, Simpson J. 3D echocardiography in congenital heart disease: a valuable tool for the surgeon. Future Cardiol 2014;10:497-509. [Crossref] [PubMed]
- Faletra FF, Ho SY, Regoli F, et al. Real-time three dimensional transoesophageal echocardiography in imaging key anatomical structures of the left atrium: potential role during atrial fibrillation ablation. Heart 2013;99:133-42. [Crossref] [PubMed]
- Aggeli C, Felekos I, Kastellanos S, et al. Real-time three-dimensional echocardiography: never before clinical efficacy looked so picturesque. Int J Cardiol 2015;198:15-21. [Crossref] [PubMed]
- Roberson DA, Cui VW. Three-dimensional transesophageal echocardiography of atrial septal defect device closure. Curr Cardiol Rep 2014;16:453. [Crossref] [PubMed]
- Shiota T. Clinical application of 3-dimensional echocardiography in the USA. Circ J 2015;79:2287-98. [Crossref] [PubMed]
- Hascoët S, Warin-Fresse K, Baruteau AE, et al. Cardiac imaging of congenital heart diseases during interventional procedures continues to evolve: Pros and cons of the main techniques. Arch Cardiovasc Dis 2016;109:128-42. [Crossref] [PubMed]
- Camargo GC, Anzanello MX, Silva RM, et al. X-shaped secundum atrial septal defect seen by 3-dimensional echocardiography: comparison with open-heart view. J Am Coll Cardiol 2014;63:693. [Crossref] [PubMed]
- Aubry P, Brochet E, Verdonk C, et al. 3-D transoesophageal echocardiography guidance in percutaneous closure of three distant atrial septal defects. Eur Heart J Cardiovasc Imaging 2015;16:1045. [Crossref] [PubMed]
- Faletra FF, Ramamurthi A, Dequarti MC, et al. Artifacts in three-dimensional transesophageal echocardiography. J Am Soc Echocardiogr 2014;27:453-62. [Crossref] [PubMed]
Cite this article as: Turner TC, Means G, Weickert T, Vavalle JP. The role of real time 3D-transesophageal echocardiography for safe and successful atrial septal defect closure. J Xiangya Med 2019;4:19.


