Update on coronectomy
Introduction
Mandibular third molars (M3M) are the most commonly impacted teeth (1). Removing M3Ms is a challenging surgical procedure due to close proximity to anatomical structures such as the inferior alveolar nerve (IAN) and lingual nerves. IAN injury (IANI) should be prevented where possible as trigeminal sensory neuropathies result in long term chronic pain and disability for 70% of patients affected (2).
Coronectomy (partial tooth removal, deliberate vital root retention and partial odontectomy) has become a routine oral surgical procedure with the aim to minimise risk of IANI in relation to the removal of high-risk M3Ms. Coronectomy, a coded surgical procedure both in US (OMFS Category service 2 D7251) and Japan, has been defined as a method of removing the crown of a tooth but leaving the roots untouched, which may be intimately related with the IAN, so that the possibility of nerve injury is reduced. At the inception of this technique questions were raised (3). and despite its increasing popularity and acceptance, there are many concerns.
The main justification for considering a coronectomy is based upon the assessed risk of IANI related to M3M surgery. Neurosensory impairment is a common complication of extraction of impacted M3Ms, and the incidence ranges from 0.35% to 8.4% (4-6). The consequences of sensory nerve injury are unpleasant and result in a negative effect on patient’s life, often with medicolegal repercussions.
The IANI, may occur a due to direct or indirect trauma during M3M removal (7). For example, it may result from direct compression of the nerve by instruments or the elevated roots. The IAN may also be damaged by rotating instruments used for the surgical procedure and in relation to IAN regional anaesthetic block injections (8,9). The IANI incidence varies depending upon the level of M3M anatomical risk, operative technique and following management (9-23).
Recognised factors associated with an increase the risk of IANI related to M3M surgery include; patients over the age of 25 years (24,25). This has led to recommendations for M3M early interventional surgery (14). Females have been reported to be more at risk of persistent IANI (20). The prevalence of IANI is also dependent on the surgeon experience and the methods used (24-26). A literature review of 32 prospective articles (24) highlighted that unerupted M3M status was the strongest indicator for IANI and impaction of the M3M may be associated with IANI (20). Intra-operative nerve exposure during surgery increase the risk of postoperative paraesthesia (12). IAN bleed during surgery is also reported to be associated with increased IANI (19).
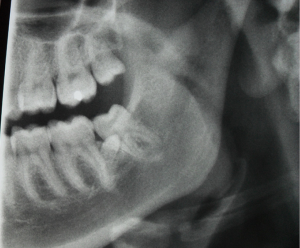
The radiographic position of the M3M in relationship to the inferior dental canal (IDC) has been shown to be useful in assessing the risk of damage to the IAN following extraction. Plane film radiographic signs on panorals indicative of possible IAN risk include:
- Roots of tooth crossing the superior border of the IDC (17-19) (Figure 1);
- Diversion of the IDC (darkening of the root) (27) (Figure 2);
- Interruption of the lamina dura (LD) (28,29) (Figure 3);
- Juxta apical area (29) (Figure 4);
- The narrowing of the root was the most significant type of superimposition, followed by dark and bifid apexes of the root (27).
Most studies (4,28-47) report a combination of panoral risk factors predisposing to IANI. However, the presence or absence of these radiographic signs does not always determine the possibility of IANI, indicating that the panoral does not have high diagnostic accuracy in the assessment of risk in surgical extractions of lower M3Ms (48,49). When the radiological marker on the panoral indicates that there is a close relationship between the M3M and the IDC, additional investigation using computed tomography (CT) may be recommended to verify the relationship in a three-dimensional (3D) view (36-51). This 3D imaging allows the surgeon to further scrutinise the need for modified surgery or intentional coronectomy (10) potentially resulting in a change of practice in up to 90–95% of cases (removal rather than coronectomy). There is limited evidence base that use of cone-beam computed tomography (CBCT) leads to reduced nerve injury despite some reports state using CBCT will reduce the morbidity to the IAN (39,40). The software associated with CBCT provides better imaging quality of M3Ms and their surrounding structures compared with conventional hospital-grade CT scans (52-54). However, CBCT has higher radiation dose and added expense compared with panoral.
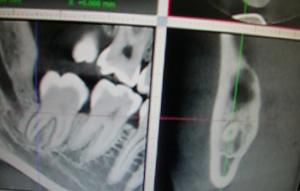
Several CBCT radiographic signs have been reported to associated with higher risk to the IAN and assist the clinician in case selection for coronectomy (55).
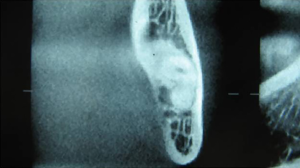
- M3M root perforation by the IDC: If the tooth is perforated, though rare, a CBCT will confirm this thus avoiding unnecessary nerve injury during extraction and lead to recommendation of a coronectomy (56);
- IDC perforation or loss of LD: Shahidi et al. (2013) (57) reported that the loss or interruption of the cortical line (LD) on the panoral, having a close correlation with proximity of the IAN to the M3M confirmed on a CBCT scan. This is “highly suggestive of the risk of nerve injury”. Also, an IDC’s LD perforation, as seen on a CBCT scan the relationship can be closely correlated to darkening of the root seen on a panoral (Figure 5) (51);
- LD interruption by the root(s) or crown of the M3M (37-40). Monaco et al. (2004) stated that the risk of IAN injury increased from the average of 1–5% to 20–30% when the IDC LD interruption by roots was observed (51);
- The length of the IDC perforation or defect depends on: the impaction depth and angulation of a M3M (37): An IDC cortical defect length (distance) of at least 3 mm on CT scan has been associated with an increased risk for intraoperative IAN exposure;
- Deformation of the IDC at the point of contact with a M3M roots (Figure 6) may indicate proximity and risk of IANI. The intimate proximity of a M3M can modify the common oval configuration of the IDC toward a more “dumbbell” or “tear-drop” shape or a concave configuration (58). Invagination of the IDC—“compression” (concave deformation) of the IDC resulting from the proximity of root(s) of a M3M. In a second study, among 169 M3Ms (115 patients), IAN injury was observed in 13 of 169 M3Ms (7.7%) and in all 13 cases with IAN injury exhibited absence of cortication. A dumb-bell-shaped IDC was considered a useful predictor for IANI [sensitivity, 69.2%; specificity, 84.6% (P=0.005)] (25);
- CBCT prediction of nerve exposure: in a study comprised by Neves et al. (2012) (47), in all 14 cases where IAN was exposed during surgery, the preoperative assessment by multi-detector computed tomography (MDCT) images classified the relationship between the roots of the M3Ms and the IDC as at-risk (the tooth roots invade and restrict the IDC space). There was a statistically significant relationship between IAN exposure and the relationship between the roots of the M3Ms and the IDC (P=0.015);
- Bifid IDCs are common in the M3M region (40): Care must be taken to carefully scrutinize the presence of bifid IDCs as often a smaller branch may be passing close to the M3M roots and on extraction will cause partial permanent IANI (44);
- M3M roots “positioned between missing lingual cortex and IDC. Thirty percent of high risk M3M cases are reported to have a defect of the lingual cortex (40), if the M3M root is sandwiched between the IDC and lost lingual cortex this may be a secondary decision factor to undertake a coronectomy (10);
- Buccal position of roots in contact with a lingually placed IDC may be associated with increased IANI rate (Figure 7) (41,59).
As yet there are no evidence-based criteria to indicate the need of a CBCT based upon panoral findings. The M3M roots should be proximal to (touching/passing roof or and floor) IDC with following features which correlate with CBCT identification of IDC proximity and M3M roots (60).
- Darkening of M3M root only or with;
- Diversion of IDC by M3M root;
- Deflected M3M root by IDC.
Consideration of how CBCT may impact on patient selection for coronectomy assumes that if 100 patients display afore mentioned risk indices on a panoral, then 98 of the 100 patients will experience no permanent IANI on M3M removal, based upon the evidence presented. Thus, if all the patients undergo coronectomy, based upon panoral films, 98% of patients will have undergone inappropriate surgery as it is ideally indicated only the 2% patients likely to get the permanent nerve injury.
Therefore, I suggest that further risk assessment using CBCT must optimise treatment planning and restricting prescription of coronectomy only to the cohort of patients at risk of permanent IANI (2%). Based upon the argument above then in my opinion all patients, identified at high risk on panoral, should undergo CBCT (as lower radiation dose as possible). However, it may not always be possible to have physical or financial access to CBCT for risk assessment prior to M3M surgery. If a patient is at obvious risk based upon the panoral findings, a decision should be agreed between patient and clinician as to whether a coronectomy should be undertaken, based upon the full understanding the related risks of coronectomy as against the preferred removal of the M3M.
Indications for coronectomy are based upon several criteria including;
- When there is an indication for extraction;
- The tooth in question has been identified as “High risk” of IANI (M3M or other teeth) (CBCT risk factors listed in Table 1 and Plain film risk factors listed in Table 2);
Table 1
CBCT features that may lead to increased risk of nerve injury on removal of the M3M and lead to consideration of coronectomyTooth root perforation by IDC: the “polo minted” tooth is the single unambiguous indicator for coronectomy. This is a rare phenomenon but increased in the Asian population (27-47) Lingual Position of the IDC in relation to the M3M root Direct contact is reported to be significantly associated with IANI but usually in relation to additional CBCT findings. Multivariate analysis showed narrowing of the IAN IDC to be the strongest independent predictors of IANI (39) Decortication: a cortical defect size ≥3 mm was associated with an increased risk for intraoperative IAN visualization with a high sensitivity and specificity (≥0.82) (37) Altered shape of IDC: CBCT influenced the treatment plan for 12%. Direct contact in combination with narrowing of the IDC lumen and IDC positioned in a bending or a groove in the root complex observed in CBCT images were significant factors for deciding on coronectomy (39,46) Loss of lingual cortex occurs frequently (30%) and may be a second indication for undertaking coronectomy if a root is positioned between the missing lingual cortex and the IDC (40) M3M, mandibular third molar; IDC, inferior dental canal; IANI, inferior alveolar nerve injury; CBCT, cone-beam computed tomography.Table 2
Radiographic signs that may indicate higher risk of IANI where roots of the M3M are in close proximity with the IDC on panoralPlain radiographic signs indicative of possible IAN risk include: Diversion of the IDC Darkening of the root Narrowing of the root/IDC Interruption of the IDC lamina dura. Interruption of the juxta‐apical area CBCT radiographic signs if increased risk to IAN Loss of IDC cortex (>3 mm) Dumb bell distortion of IDC Lingual position of IDC to roots Perforation of tooth roots by IDC Inter radicular IDC with multiple roots M3M, mandibular third molar; IDC, inferior dental canal; IANI, inferior alveolar nerve injury; CBCT, cone-beam computed tomography. - The patient is healthy (medical history and social follow-up accessibility);
- Dental (vital tooth).
Contraindications for coronectomy include;
- Dental factors;
- Non-vital tooth;
- Active caries into the pulp or demonstrating periapical abnormality;
- M3Ms that are mobile should be excluded as they act as a mobile foreign body and become a nidus for infection or migration;
- M3Ms associated with tumours;
- Horizontally impacted M3Ms more difficult to obtain a successful coronectomy due to high placement of the retained root surface in relation to the alveolus.
- Medical history immune compromised with likely poor healing is a contraindication for coronectomy and removal is advised where bye the patient may be more at risk of infection with retention of roots;
- Social and psychological factors.
- The patient’s understanding is compromised;
- Travelling/difficult access to healthcare;
- Specific indications to remove the tooth: avoidance of third molar surgery will avoid nerve injury, which is possible for non-diseased unerupted M3Ms in accordance with AAOMS 2016 guidelines recommending active surveillance for 23% of M3Ms (http://www.aaoms.org/docs/govt_affairs/advocacy_white_papers/management_third_molar_white_paper.pdf);
- Patients scheduled for future surgery involving the site.
When should the surgeon consider undertaking a coronectomy? Some possible indications are listed in Tables 1,2. There are complications related to coronectomy which leads to complex consent processes and requires detailed explanation for informed patient consent. Recent systematic reviews (61,62) have evaluated the clinical effectiveness of the surgical technique of coronectomy for M3M extraction in close proximity with the IAN. The authors assessed the following variables: IANI, lingual nerve injury, postoperative adverse effects, pulp disease, root migration and rate of reoperation. Ten articles qualified for the final analysis. The successful coronectomies varied from a minimum of 61.7% to a maximum of 100%. Coronectomy was associated with a low incidence of complications in terms of IANIs (0–9.5%), lingual nerve injury (0–2%), postoperative pain (1.1–41.9%) and swelling (4.6%), dry socket symptoms (2–12%), infection rate (1–9.5%) and pulp disease (0.9%). Migration of the M3M retained roots seems to be a frequent occurrence (2–85.3%). Their conclusion was that coronectomy appears to be a safe procedure at least in the short term, with a reduced incidence of postoperative complications.
A further systematic review (63) of four studies indicated that the pooled risk ratio (coronectomy vs. total removal). The authors therefore concluded that, coronectomy appears superior to total removal for reducing IAN damage and could be used in clinical practice for third molar extractions with high risk of nerve injury.
- “Dry socket” symptoms and infection: Rates for socket infection (2–12%), infection rate (1–9.5%) and pulp disease (0.9%) were reported in a systematic review of four studies (63). Two randomized controlled trial involving coronectomies and controls reported a significantly lower pain and “dry socket” incidence in the coronectomy group (64,65);
- IANI deficit: Lower incidence of IANIs is reported for coronectomy compared to complete extraction of M3M (65-70). Leung and Cheung (2010) (64) reported a 0.65% IANI rate for coronectomy versus 5.10% removal;
- Failed coronectomy: Renton et al. (2005) (65) reported a high failed coronectomy rate with intraoperative mobilization of the tooth roots on separating the M3M crown from the roots intra-operatively. As a result, the technique has been modified. This study preceded CBCT and when a M3M is identified as high risk based upon CBCT the crown section is less minimal than for an extraction procedure but sufficient to ensure separation of the crown from the roots without mobilizing the roots;
- Enamel retention: a repeat coronectomy is recommended for cases in which enamel retention is diagnosed in order to prevent residual roots from becoming infected (71);
- Root migration with eruption: migration of the roots was identified in 80% of 116 patients and was increased in younger patients (64). Three percent at 3 years eruption and necessary removal has been reported (64). A study of coronectomies undertaken in 64 patients (72), reported that the most common complication was tooth migration away from the mandibular IDC (n=14), followed by root exposure (n=5). Re-operation to remove the root was performed in cases with periapical infection and root exposure. Migration of the roots was found more commonly in younger patients and within the first 6 months post-surgery (73);
- Reoperation rates.
- Late extraction due to root migration is reported in many studies. Extraction in 3.6% cases was necessary due to late eruption (74) and 6% (75). On removal of these roots one study reported that there was no pathology associated with retained roots when removed (76);
- Repeat coronectomy is reported and successful if enamel remnants require removal (71);
- Reoperation in 20 cases (3.26%) were reoperated on to.
- Remove residual enamel [2];
- Chronic infection [2];
- Root exposure [13] and roots removed (2.12%);
- Vague pain [2] resulting in roots being removed;
- One case required orthognathic surgery and root was removed (73).
Legal issues
Coronectomy is an accepted and emerging technique. Currently, 3 National M3M Guidance include coronectomy as a treatment option, however, there was a National Health Service Litigation Authority (NHSLA) case (2009) that concluded that it was a breach of duty not to offer a patient with high risk M3M further risk assessment and or a coronectomy (77).
Patient consent is complex for coronectomy and time should be taken to explain the risks and benefits of the procedure. The surgeon must be primarily responsible for the presurgical assessment and as a result must be competent in reading the CBCT and reporting the risk assessment. There are additional issues regarding CBCT including radiographic reporting of a large anatomical area and the legal responsibilities of both clinician and radiologist (78). The surgeon must be appropriately trained in the technique, incidence of IANI and LNI would not occur if the procedure is appropriately undertaken. In addition, the internet is peppered with poor surgical practice videos of coronectomy using high-speed drills, half sectioning the enamel crown and complete sectioning of the crown which is more likely to lead to lingual nerve injury.
Lastly there is insufficient evidence to state that CBCT reduces IANIs. However, reports claim that due to the high variability of the anatomical relationship in case of high-risk M3Ms, a CBCT scan should be performed for thorough case planning (60). Furthermore, using CBCT will avoid unnecessary coronectomies thus increasing removal without nerve injury, which is the optimum possible treatment. Over 30% of high-risk M3Ms as seen on panoral radiography are found to be distant from the IDC on CBCT and therefore should be extracted (60). Further research is required to ascertain the benefit of CBCT in these cases. Renton et al. (2005) (65) described a change in practice of over 95% of cases based upon CBCT findings resulting in only 5% of M3Ms undergoing coronectomy. If patient is unsuitable or the M3M is carious, thus extraction is indicated, (CBCT can offer an excellent planning tool to minimize risk to IAN when planning surgery, the evidences, to support this practice is emerging.
Recommendations
Coronectomy is an effective and accepted method for minimising IANIs related to the management of high-risk M3Ms (79). However, explicit criteria for requesting a CBCT based on risk assessment of the panoral are not yet absolutely clear. Nor are there explicit criteria for recommending a coronectomy based on CBCT findings as yet. This leaves a degree of ambiguity and uncertainty in prescribing coronectomy rather than extraction for M3Ms
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editor (Zaid H. Baqain) for the series “Oral and Maxillofacial Surgery” published in Journal of Xiangya Medicine. The article has undergone external peer review.
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2018.07.01). The series “Oral and Maxillofacial Surgery” was commissioned by the editorial office without any funding or sponsorship. The author has no other conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).The study received approval from the Institutional Board Review Committee of Tulane University (No. 351684-OTH) with a waiver of written informed consent.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Celikoglu M, Miloglu O, Kazanci F. Frequency of agenesis, impaction, angulation, and related pathologic changes of third molar teeth in orthodontic patients. J Oral Maxillofac Surg 2010;68:990-5. [Crossref] [PubMed]
- Renton T, Yilmaz Z. Profiling of patients presenting with posttraumatic neuropathy of the trigeminal nerve. J Orofac Pain 2011;25:333-44. [PubMed]
- Assael LA. Coronectomy: a time to ponder or a time to act? J Oral Maxillofac Surg 2004;62:1445-6. [Crossref] [PubMed]
- Cheung LK, Leung YY, Chow LK, et al. Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg 2010;39:320-6. [Crossref] [PubMed]
- Haug RH, Perrott DH, Gonzalez ML, et al. The American Association of Oral and Maxillofacial Surgeons Age-Related Third Molar Study. J Oral Maxillofac Surg 2005;63:1106-14. [Crossref] [PubMed]
- Lopes V, Mumenya R, Feinmann C, et al. Third molar surgery: an audit of the indications for surgery, post-operative complaints and patient satisfaction. Br J Oral Maxillofac Surg 1995;33:33-5. [Crossref] [PubMed]
- Gerlach KL, Hoffmeister B, Walz C. Dysesthesia and anesthesia of the mandibular nerve following dental treatment. Dtsch Zahnarztl Z 1989;44:970-2. [PubMed]
- Renton T. Oral surgery: part 4. Minimising and managing nerve injuries and other complications. Br Dent J 2013;215:393-9. [Crossref] [PubMed]
- Kipp DP, Goldstein BH, Weiss WW Jr. Dysesthesia after mandibular third molar surgery: a retrospective study and analysis of 1,377 surgical procedures. J Am Dent Assoc 1980;100:185-92. [Crossref] [PubMed]
- Black CG. Sensory impairment following lower third molar surgery: a prospective study in New Zealand. N Z Dent J 1997;93:68-71. [PubMed]
- Gülicher D, Gerlach KL. Sensory impairment of the lingual and inferior alveolar nerves following removal of impacted mandibular third molars. Int J Oral Maxillofac Surg 2001;30:306-12. [Crossref] [PubMed]
- Tay AB, Go WS. Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg 2004;62:592-600. [Crossref] [PubMed]
- Queral-Godoy E, Valmaseda-Castellon E, Berini-Aytes L, et al. Incidence and evolution of inferior alveolar nerve lesions following lower third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:259-64. [Crossref] [PubMed]
- Blondeau F, Daniel NG. Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Can Dent Assoc 2007;73:325. [PubMed]
- Ghaeminia H, Meijer GJ, Soehardi A, et al. Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoraly. Int J Oral Maxillofac Surg 2009;38:964-71. [Crossref] [PubMed]
- Szalma J, Lempel E, Jeges S, et al. Darkening of third molar roots: panoralic associations with inferior alveolar nerve exposure. J Oral Maxillofac Surg 2011;69:1544-9. [Crossref] [PubMed]
- Kim JW, Cha IH, Kim SJ, et al. Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral Maxillofac Surg 2012;70:2508-14. [Crossref] [PubMed]
- Guerrero ME, Nackaerts O, Beinsberger J, et al. Inferior alveolar nerve sensory disturbance after impacted mandibular third molar evaluation using cone beam computed tomography and panoraly: a pilot study. J Oral Maxillofac Surg 2012;70:2264-70. [Crossref] [PubMed]
- Smith WP. The relative risk of neurosensory deficit following removal of mandibular third molar teeth: the influence of radiography and surgical technique. Oral Surg Oral Med Oral Pathol Oral Radiol 2013;115:18-24. [Crossref] [PubMed]
- Selvi F, Dodson TB, Nattestad A, et al. Factors that are associated with injury to the inferior alveolar nerve in high-risk patients after removal of third molars. Br J Oral Maxillofac Surg 2013;51:868-73. [Crossref] [PubMed]
- Nguyen E, Grubor D, Chandu A. Risk factors for permanent injury of inferior alveolar and lingual nerves during third molar surgery. J Oral Maxillofac Surg 2014;72:2394-401. [Crossref] [PubMed]
- Deppe H, Mucke T, Wagenpfeil S, et al. Trigeminal nerve injuries after mandibular oral surgery in a university outpatient setting--a retrospective analysis of 1,559 cases. Clin Oral Investig 2015;19:149-57. [Crossref] [PubMed]
- Jain N, Thomas S, Prabhu S, et al. Influence of tooth sectioning technique and various risk factors in reducing the IAN injury following surgical removal of an impacted mandibular third molar. Oral Maxillofac Surg 2016;20:149-56. [Crossref] [PubMed]
- Bruce RA, Frederickson GC, Small GS. Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc 1980;101:240-5. [Crossref] [PubMed]
- Adeyemo WL, Ogunlewe MO, Ladeinde AL, et al. A comparative study of surgical morbidity associated with mandibular third-molar surgery in young and aging populations. J Contemp Dent Pract 2010;11:E001-8. [PubMed]
- Piecuch JF. What strategies are helpful in the operative management of third molars? J Oral Maxillofac Surg 2012;70:S25-32. [Crossref] [PubMed]
- Hasegawa T, Ri S, Shigeta T, et al. Risk factors associated with inferior alveolar nerve injury after extraction of the mandibular third molar--a comparative study of preoperative images by panoraly and computed tomography. Int J Oral Maxillofac Surg 2013;42:843-51. [Crossref] [PubMed]
- Leung YY, Cheung LK. Correlation of radiographic signs, inferior dental nerve exposure, and deficit in third molar surgery. J Oral Maxillofac Surg 2011;69:1873-9. [Crossref] [PubMed]
- Rud J. Third molar surgery: perforation of the inferior dental nerve through the root. Tandlaegebladet 1983;87:659-67. [PubMed]
- Leung YY, Cheung LK. Risk factors of neurosensory deficits in lower third molar surgery: an literature review of prospective studies. Int J Oral Maxillofac Surg 2011;40:1-10. [Crossref] [PubMed]
- Alantar A, Roisin-Chausson MH, Commissionat Y, et al. Retention of third molar roots to prevent damage to the inferior alveolar nerve. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1995;80:126. [Crossref] [PubMed]
- Renton T, Hankins M, Sproate C, et al. A randomised controlled clinical trial to compare the incidence of injury to the inferior alveolar nerve as a result of coronectomy and removal of mandibular third molars. Br J Oral Maxillofac Surg 2005;43:7-12. [Crossref] [PubMed]
- Howe GL, Poynton HG. Prevention of damage to the inferior alveolar nerve during extraction of mandibular third molars. Br Dent J 1960;109:353-63.
- Kaeppler G. Conventional cross-sectional tomographic evaluation of mandibular third molars. Quintessence Int 2000;31:49-56. [PubMed]
- Blaeser BF, August MA, Donoff RB, et al. Panoralic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg 2003;61:417-21. [Crossref] [PubMed]
- Ohman A, Kivijarvi K, Blomback U, et al. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac Radiol 2006;35:30-5. [Crossref] [PubMed]
- Susarla SM, Sidhu HK, Avery LL, et al. Does computed tomographic assessment of inferior alveolar canal cortical integrity predict nerve exposure during third molar surgery? J Oral Maxillofac Surg 2010;68:1296-303. [Crossref] [PubMed]
- Katakam SK, Shankar U, Thakur D, et al. Comparison of orthopantomography and computed tomography image for assessing the relationship between impacted mandibular third molar and mandibular canal. J Contemp Dent Pract 2012;13:819-23. [Crossref] [PubMed]
- Eyrich G, Seifert B, Matthews F, et al. 3-Dimensional imaging for lower third molars: is there an implication for surgical removal? J Oral Maxillofac Surg 2011;69:1867-72. [Crossref] [PubMed]
- Umar G, Obisesan O, Bryant C, et al. Elimination of permanent injuries to the inferior alveolar nerve following surgical intervention of the "high risk" third molar. Br J Oral Maxillofac Surg 2013;51:353-7. [Crossref] [PubMed]
- Xu GZ, Yang C, Fan XD, et al. Anatomic relationship between impacted third mandibular molar and the mandibular canal as the risk factor of inferior alveolar nerve injury. Br J Oral Maxillofac Surg 2013;51:e215-9. [Crossref] [PubMed]
- Pathak S, Mishra N, Rastogi MK, et al. Significance of radiological variables studied on orthopantamogram to pridict post-operative inferior alveoler nerve paresthesia after third molar extraction. J Clin Diagn Res 2014;8:ZC62-4. [PubMed]
- Peker I, Sarikir C, Alkurt MT, et al. Panoraly and cone-beam computed tomography findings in preoperative examination of impacted mandibular third molars. BMC Oral Health 2014;14:71. [Crossref] [PubMed]
- Maglione M, Costantinides F, Bazzocchi G. Classification of impacted mandibular third molars on cone-beam CT images. J Clin Exp Dent 2015;7:e224-31. [Crossref] [PubMed]
- Huang CK, Lui MT, Cheng DH. Use of panoraly to predict postsurgical sensory impairment following extraction of impacted mandibular third molars. J Chin Med Assoc 2015;78:617-22. [Crossref] [PubMed]
- Matzen LH, Christensen J, Hintze H, et al. Influence of cone beam CT on treatment plan before surgical intervention of mandibular third molars and impact of radiographic factors on deciding on coronectomy vs surgical removal. Dentomaxillofac Radiol 2013;42:98870341. [Crossref] [PubMed]
- Neves FS, de Almeida SM, Boscolo FN, et al. Risk assessment of inferior alveolar neurovascular bundle by multidetector computed tomography in extractions of third molars. Surg Radiol Anat 2012;34:619-24. [Crossref] [PubMed]
- Bell GW. Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Radiological and surgical findings, and clinical outcome. Br J Oral Maxillofac Surg 2004;42:21-7. [Crossref] [PubMed]
- de Melo Albert DG, Gomes AC, do Egito Vasconcelos BC, et al. Comparison of orthopantomographs and conventional tomography images for assessing the relationship between impacted lower third molars and the mandibular canal. J Oral Maxillofac Surg 2006;64:1030-7. [Crossref] [PubMed]
- Maegawa H, Sano K, Kitagawa Y, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2003;96:639-46. [Crossref] [PubMed]
- Monaco G, Montevecchi M, Bonetti GA, et al. Reliability of panoraly in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 2004;135:312-8. [Crossref] [PubMed]
- Ludlow JB, Davies-Ludlow LE, Brooks SL, et al. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 2006;35:219-26. [Crossref] [PubMed]
- Hashimoto K, Kawashima S, Kameoka S, et al. Comparison of image validity between cone beam computed tomography for dental use and multidetector row helical computed tomography. Dentomaxillofac Radiol 2007;36:465-71. [Crossref] [PubMed]
- Loubele M, Guerrero ME, Jacobs R, et al. A comparison of jaw dimensional and quality assessments of bone characteristics with cone-beam CT, spiral tomography, and multi-slice spiral CT. Int J Oral Maxillofac Implants 2007;22:446-54. [PubMed]
- Céspedes-Sánchez JM, Ayuso-Montero R, Mari-Roig A, et al. The importance of a good evaluation in order to prevent oral nerve injuries: a review. Acta odontologica Scandinavica 2014;72:161-7. [Crossref] [PubMed]
- Pippi R. A case of inferior alveolar nerve entrapment in the roots of a partially erupted mandibular third molar. J Oral Maxillofac Surg 2010;68:1170-3. [Crossref] [PubMed]
- Shahidi S, Zamiri B, Bronoosh P. Comparison of panoraly with cone beam CT in predicting the relationship of the mandibular third molar roots to the alveolar canal. Imaging Sci Dent 2013;43:105-9. [Crossref] [PubMed]
- Tolstunov L. The quest for causes of inferior alveolar nerve injury after extraction of mandibular third molars. J Oral Maxillofac Surg 2014;72:1644-6. [Crossref] [PubMed]
- Park W, Choi JW, Kim JY, et al. Cortical integrity of the inferior alveolar canal as a predictor of paresthesia after third-molar extraction. J Am Dent Assoc 2010;141:271-8. [Crossref] [PubMed]
- Tantanapornkul W, Okochi K, Bhakdinaronk A, et al. Correlation of darkening of impacted mandibular third molar root on digital panoramic images with cone beam computed tomography findings. Dentomaxillofac Radiol 2009;38:11-6. [Crossref] [PubMed]
- Ghaeminia H. Coronectomy may be a way of managing impacted third molars. Evid Based Dent 2013;14:57-8. [Crossref] [PubMed]
- Martin A, Perinetti G, Costantinides F, et al. Coronectomy as a surgical approach to impacted mandibular third molars: a systematic review. Head Face Med 2015;11:9. [Crossref] [PubMed]
- Long H, Zhou Y, Liao L, et al. Coronectomy vs. total removal for third molar extraction: a systematic review. J Dent Res 2012;91:659-65. [Crossref] [PubMed]
- Leung YY, Cheung LK. Safety of coronectomy versus excision of wisdom teeth: a randomized controlled trial. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2009;108:821-7. [Crossref] [PubMed]
- Renton T. Update on coronectomy. A safer way to remove high risk mandibular third molars. Dent Update 2013;40:362-4, 366-8. [Crossref] [PubMed]
- Ueda M, Nakamori K, Shiratori K, et al. Clinical significance of computed tomographic assessment and anatomic features of the inferior alveolar canal as risk factors for injury of the inferior alveolar nerve at third molar surgery. J Oral Maxillofac Surg 2012;70:514-20. [Crossref] [PubMed]
- Dolanmaz D, Yildirim G, Isik K, et al. A preferable technique for protecting the inferior alveolar nerve: coronectomy. J Oral Maxillofac Surg 2009;67:1234-8. [Crossref] [PubMed]
- Hatano Y, Kurita K, Kuroiwa Y, et al. Clinical evaluations of coronectomy (intentional partial odontectomy) for mandibular third molars using dental computed tomography: a case-control study. J Oral Maxillofac Surg 2009;67:1806-14. [Crossref] [PubMed]
- O'Riordan BC. Coronectomy (intentional partial odontectomy of lower third molars). Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:274-80. [Crossref] [PubMed]
- Pogrel MA, Lee JS, Muff DF. Coronectomy: a technique to protect the inferior alveolar nerve. J Oral Maxillofac Surg 2004;62:1447-52. [Crossref] [PubMed]
- Frenkel B, Givol N, Shoshani Y. Coronectomy of the mandibular third molar: a retrospective study of 185 procedures and the decision to repeat the coronectomy in cases of failure. J Oral Maxillofac Surg 2015;73:587-94. [Crossref] [PubMed]
- Agbaje JO, Heijsters G, Salem AS, et al. Coronectomy of Deeply Impacted Lower Third Molar: Incidence of Outcomes and Complications after One Year Follow-Up. J Oral Maxillofac Res 2015;6:e1. [Crossref] [PubMed]
- Leung YY, Cheung LK. Coronectomy of the lower third molar is safe within the first 3 years. J Oral Maxillofac Surg 2012;70:1515-22. [Crossref] [PubMed]
- Leung YY, Cheung LK. Long-term morbidities of coronectomy on lower third molar. Oral Surg Oral Med Oral Pathol Oral Radiol 2016;121:5-11. [Crossref] [PubMed]
- Monaco G, De Santis G, Pulpito G, et al. What Are the Types and Frequencies of Complications Associated With Mandibular Third Molar Coronectomy? A Follow-Up Study. J Oral Maxillofac Surg 2015;73:1246-53. [Crossref] [PubMed]
- Patel V, Sproat C, Kwok J, et al. Histological evaluation of mandibular third molar roots retrieved after coronectomy. Br J Oral Maxillofac Surg 2014;52:415-9. [Crossref] [PubMed]
- R (on the application of ELIZABETH ROSE) v Thanet Clinical Commissioning Group [2014] EWHC 1182 (Admin)
- Dawood A, Patel S, Brown J. Cone beam CT in dental practice. Br Dent J 2009;207:23-8. [Crossref] [PubMed]
- Cervera-Espert J, Pérez-Martínez S, Cervera-Ballester J, et al. Coronectomy of impacted mandibular third molars: A meta-analysis and systematic review of the literature. Med Oral Patol Oral Cir Bucal 2016;21:e505-13. [PubMed]
Cite this article as: Renton T. Update on coronectomy. J Xiangya Med 2018;3:30.