
Imaging by multislice CT of a large aortico-left ventricular tunnel mimicking as ventricular septal defect
Introduction
Aortico-left ventricular tunnel (ALVT) is a very rare congenital heart disease that presents as an abnormal paravalvular communication between the left ventricle and ascending aorta. It was originally described in 1961 (1). Here we describe a large aneurysmally dilated tunnel which masqueraded as a ventricular septal defect (VSD) on echocardiography. This was correctly diagnosed as ALVT on multislice CT. The dilated aneurysmal portion was compressing the right ventricular outflow tract and was lying in the region of right ventricle and all this resulted in its being labeled as VSD on echocardiography. This report highlights the significance of multislice CT angiography (CTA) in accurate preoperative diagnosis of this rare entity. Early diagnosis is essential to prevent heart failure.
Case presentation
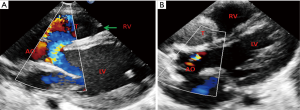
A 1-month-old baby with features of congestive heart failure was admitted. Echocardiography suspected a large subaortic VSD with enlarged left ventricle but normal function. On echocardiogram, there was suggestion of possible diastolic murmur with mild to moderate aortic regurgitation. Right ventricle was adequate in size. There was no atrial septal defect, patent ductus arteriosus or coarctation of aorta. Coronary anatomy was not well seen. Due to the complex anatomy CTA was ordered. ECG-gated retrospective CTA with tube current modulation was performed using Omnipaque (350 mgI/mL) at a rate of 3 mL/kg followed by a saline flush. It revealed a large extra-cardiac communication between the aorta and the left ventricle. The lesion arose from above the right coronary sinus (RCS) of Valsalva at the level of sinotubular junction and was seen to communicate with the left ventricular outflow tract at its distal end. The right coronary artery ostium was well away from the origin of the tunnel. Following a post-ostial narrowing, there was an aneurysmally dilated segment above and it was compressing the right ventricular outflow tract (Figures 1,2; Figure S1). The aneurysmal segment was compressing the right ventricle. No VSD was noted. A diagnosis of type two ALVT was made. The echocardiographic diagnosis of VSD was likely due to the aneurysmally dilated segment masquerading as the right ventricle. The child underwent operative repair. The aneurysmal sac was opened through RCS and distal opening into left ventricle was closed with Gore-Tex patch. Subsequently the aneurysmal sac was closed over the patch.

Several theories have been put forward trying to explain the etiology of ALVT including bulbus cordis malformation, abnormality in anterior aortic wall leading to communication with left ventricle, aberrant coronary artery dissection, persistent fifth aortic arch to name a few (2,3). However, the exact cause still remains unknown.
Discussion
Incidence
ALVT is an extremely rare congenital anomaly with a reported incidence of 0.001% with a male preponderance (4). Aortico-right ventricular tunnel is an even rare entity accounting for approximately 10% of all cases (5).
Clinical profile
Most cases present early with features of congestive heart failure and aortic regurgitation. The mechanism behind aortic regurgitation may include deficient support in aortic root, damage to leaflets by the turbulent jet, or congenital valve abnormalities. The tunnel separates aortic root and right cusp from the ventricular septum leading to aortic insufficiency (6). Presence of severe aortic insufficiency in infants should raise suspicion of ALVT. The symptom severity correlates with the cross-sectional area of the tunnel (7). Left ventricle volume overload is seen in large tunnels while if small the patient may survive into adulthood without repair (3). It manifests between ascending aorta and left ventricle as an extra-cardiac paravalvular tunnel. More often it arises above the RCS of Valsalva with an anterolateral location of tunnel in relation to ascending aorta (8). Rarely, it may arise above left sinus of Valsalva and has a more benign course as this travels through myocardium to reach left ventricle that limits the rate of enlargement and subsequent heart failure (3).
Echocardiography and invasive catheter angiography have been used in the past for the diagnosis. However, multislice CTA clearly depicts the ALVT, identifies associated cardiac anomalies like VSD, patent foramen ovale, aortic stenosis, patent ductus arteriosus, bicuspid aortic valve and pulmonary stenosis as well as coronary artery anomalies like absent coronary artery ostium, absent right coronary artery or the ostium may lie within the tunnel (9). CTA is valuable in differentiation from other lesions that can mimic the diagnosis (VSD, ruptured sinus of Valsalva aneurysm and coronary artery fistula). In sinus of Valsalva aneurysm, the lesion involves coronary sinus of Valsalva but in ALVT it arises just above the sinotubular junction (10).
Types of ALVT
ALVT comprises four anatomical types as described by Hovaguimian et al. (I) slit-like aortic orifice with no evidence of valvular distortion; (II) large oval shaped aortic orifice with an aneurysmal extracardiac component; (III) intracardiac aneurysmal component with an oval orifice; (IV) it’s a combination of type 2 and 3 (11). These subtypes are well depicted by multislice CT. Besides, three-dimensional reconstructions on CT assist in optimal surgical planning.
Treatment
Early surgical repair is recommended due to risk of the development of aortic regurgitation in patients who are operated later (12). Various surgical closure techniques include patch closure, direct closure and closure of both the aortic and ventricular ends of tunnel with obliteration of the tunnel (13). Patients with slit like opening may be managed by mattress or continuous suture. In cases with large aortic opening, patch closure is advised to prevent valvular distortion as in our case (11). Patch closure stabilizes the right coronary cusp to its position and prevents aortic regurgitation and is thus recommended (14). Direct closure of ventricular orifice is not recommended as it is not surrounded by muscular myocardium (15). Percutaneous closure using Amplatzer occluder device has also been advocated (7,16). It may work best if the tunnel is located far away from the coronary ostia with no significant aortic valve distortion and aortic insufficiency. Medical management is only for symptomatic relief of heart failure.
Follow-up
Post-operative period requires careful observation for any development of aortic regurgitation, the incidence of which varies from 16% to 60% (17). More than half of patients may eventually require a valve replacement (18,19). The acquired aortic insufficiency may be due to progressive aortic root dilation, or leaflet perforation secondary to hemodynamic trauma.
Conclusions
ALVT is an extremely rare diagnosis presenting as congestive heart failure in infancy. Echocardiography is the first line of modality. However due to its highly operator dependence, the complicated anatomy can be missed sometimes like in our case. Multislice CTA provides the detailed and accurate preoperative anatomy including information about coronaries and other unforeseen extracardiac anomalies. Thus use of CTA is highly desirable in difficult cases.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.11.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Edwards JE. Aneurysm of thoracic aorta. In: Atlas of Acquired Diseases of the Heart and Great Vessels. 2nd ed. Philadelphia: W.B. Saunders Company, 1961:1142.
- Li D, Yan J, Shen X, et al. Surgical treatment of aortico-left ventricular tunnel: a 12-year experience. Cardiology 2009;114:150-6. [Crossref] [PubMed]
- Kim RW, Spray TL. Surgical correction of aortico-left ventricular tunnel. Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2006;177-9. [Crossref] [PubMed]
- Martins JD, Sherwood MC, Mayer JE Jr, et al. Aortico-left ventricular tunnel: 35-year experience. J Am Coll Cardiol 2004;44:446-50. [Crossref] [PubMed]
- McKay R. Aorto-ventricular tunnel. Orphanet J Rare Dis 2007;2:41. [Crossref] [PubMed]
- Tuna IC, Edwards JE. Aortico-left ventricular tunnel and aortic insufficiency. Ann Thorac Surg 1988;45:5-6. [Crossref] [PubMed]
- Kathare P, Subramanyam RG, Dash TK, et al. Diagnosis and management of aorto-left ventricular tunnel. Ann Pediatr Cardiol 2015;8:103-7. [Crossref] [PubMed]
- Ono M, Goerler H, Boethig D, et al. Surgical repair of aortico-left ventricular tunnel arising from the left aortic sinus. Interact Cardiovasc Thorac Surg 2008;7:510-1. [Crossref] [PubMed]
- Llorens R, Arcas R, Herreros J, et al. Aortico-left ventricular tunnel: a case report and review of the literature. Tex Heart Inst J 1982;9:169-75. [PubMed]
- Song L, Jin J, Tao L. Surgical correction of an aortico-left ventricular tunnel originating from the left aortic sinus with a left coronary artery anomaly. J Card Surg 2015;30:108-10. [Crossref] [PubMed]
- Hovaguimian H, Cobanoglu A, Starr A. Aortico-left ventricular tunnel: a clinical review and new surgical classification. Ann Thorac Surg 1988;45:106-12. [Crossref] [PubMed]
- Sousa-Uva M, Touchot A, Fermont L, et al. Aortico-left ventricular tunnel in fetuses and infantS Ann Thorac Surg 1996;61:1805-10. [Crossref] [PubMed]
- Levy MJ, Schachner A, Blieden LC. Aortico-left ventricular tunnel: collective review. J Thorac Cardiovasc Surg 1982;84:102-9. [PubMed]
- Grunenfelder J, Zund G, Prêtre R, et al. Right coronary artery from aorto-left ventricular tunnel: case report of a new surgical approach. J Thorac Cardiovasc Surg 1998;116:363-5. [Crossref] [PubMed]
- Ho SY, Muriago M, Cook AC, et al. Surgical anatomy of aorto-left ventricular tunnel. Ann Thorac Surg 1998;65:509-14. [Crossref] [PubMed]
- Chessa M, Chaudhari M, De Giovanni JV. Aorto-left ventricular tunnel: transcatheter closure using an amplatzer duct occluder device. Am J Cardiol 2000;86:253-4. [Crossref] [PubMed]
- Hruda J, Hazekamp MG, Sobotka-Plojhar MA, et al. Repair of aorto-right ventricular tunnel with pulmonary stenosis and an anomalous origin of the left coronary artery. Eur J Cardiothorac Surg 2002;21:1123-5. [Crossref] [PubMed]
- Meldrum-Hanna W, Schroff R, Ross DN. Aortico-left ventricular tunnel: late follow-up. Ann Thorac Surg 1986;42:304-6. [Crossref] [PubMed]
- Serino W, Andrade JL, Ross D, et al. Aorto-left ventricular communication after closure. Late postoperative problems. Br Heart J 1983;49:501-6. [Crossref] [PubMed]
- Priya S, Gulati GS, Saxena A, et al. The axial cine image shows a large channel arising from proximal ascending aorta just above the right aortic sinus which is seen to communicate with the left ventricular outflow tract at its distal end. Asvide 2018;5:008. Available online: http://asvidett.amegroups.com/article/view/22309
Cite this article as: Priya S, Gulati GS, Saxena A, Airan B. Imaging by multislice CT of a large aortico-left ventricular tunnel mimicking as ventricular septal defect. J Xiangya Med 2018;3:3.


