Management of air leaks after thoracic surgery: old style or digital drainage?
Prolonged air leak (PAL) is one of the most common complications after pulmonary resection (1). It is defined as air coming out of the operated lung until seventh, fifth or fourth postoperative day, according to different definitions (2-5) and it is often associated with postoperative complications, causing higher hospital costs (3).
The duration of chest drain after lung resection is related to many factors and the possible inter-observer variability on presence or entity of air leak is often one of the most conditioning variable (6). The use of digital devices made possible to reduce this variability (7); several studies demonstrated their superiority compared to traditional devices (8-12), while others did not reach the same result (13).
Significant attention to details is necessary for reducing morbidity and mortality in patients submitted to lung resection; the ideal drainage of air and fluids from chest cavity as well as careful report of those data is probably one of the most important aspects of this care (14).
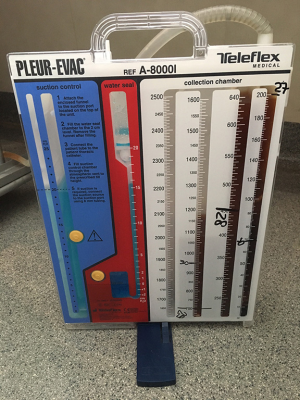
The quantification of postoperative air leaks usually relies on a visual scale, being inherently prone to subjective interpretation and inter observer variations; for this reason several companies have manufactured pleural drainage units that—thanks to electronic components—allow the digital quantification of air leaks and fluid drainage (Figure 1) (15).
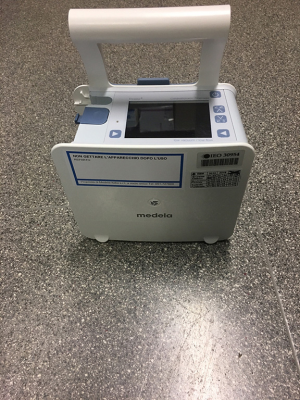
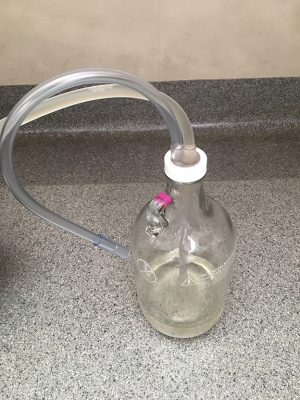
Standard analogic systems present a first chamber for fluid collection, a second chamber functioning as “water-seal” and a third chamber as suction control in case aspiration is needed; newer drainage systems do not rely on the water seal system but use a mechanical check-valve, being smaller and allowing patient discharge at home with the drainage, if indicated (Figures 2,3).
The target of digital systems is to make more objective air leak evaluation and to optimize chest tube management for a faster and safer removal.
Digital drainage is usually lightweight and compact; it has an integrated suction source and rechargeable battery, allowing the patients to ambulate without needing to be attached to wall suction. It provides digital real-time data and a 24-hour trend of the air leak, that can be transferred to a computer and included in the patient’s records. There are usually alarms that alert clinical personnel for prompt intervention in case of irregularities; moreover, digital drainage continually monitors and regulates the negative pressure close to the patient's chest, preventing the common problems such as siphons, clogs and kinks. Due to this assessment, digital drainages can be positioned at the level of the patient's chest, if needed, for example during ambulance transport. The system’s dual lumen tubing provides continuous monitoring of pressure and evacuation of fluids and air; for the collection of fluids there are usually disposable canisters with different capacities ranging from 0.3 to 2.0 liters. There is a docking station that can be placed on a level surface or be attached to a standard rail. More mobile patients can use the carrying strap placed across the shoulder, leaving their hands free (16).
Miller et al. compared postoperative course of 108 patients receiving video-assisted lobectomy or segmentectomy managed with overnight suction followed by gravity drainage in both the standard and digital drainage systems, disclosing that patients receiving VATS lung resections managed postoperatively with a digital drainage system had less morbidity and decreased hospitalization (14). However, the authors themselves describe a major concern about the cost of the disposable devices compared with the cost savings that the digital system may offer; it would be correct to determine which patients should be considered for digital drainage system, considering his preoperative risk factor. Usually the digital system is not properly indicated for sublobar resections or pleural procedures—where air leak should be extremely low and clinically irrelevant (14), as well as for standard or extended pneumonectomies—where air leak should be zero, except in case of bronchopleural fistula (17,18).
Although there was a lack of evidence about the use of pleural suction to optimize lung re-expansion after pulmonary resection (19), Leo et al. disclosed that the routine use of external pleural suction reduces PALs after standard lung resection (20); this represents a clear advantage of digital systems allowing continuous pleural suction application without forcing the patient close to the aspiration system in his room.
Takamochi et al. recently reported results from a prospective study enrolling 240 operated patients monitored by digital system to evaluate peak air leakage during the first 24 hours after the resection, patterns of air leaks during the first 72 hours and patterns of pleural pressure variations until the drainages were removed: they demonstrated that PALs can be predicted based on forced expiratory volume in the 1st second (FEV1), peak air leak in the first 24 hours following resection, and the pattern of air leak during the first 72 hours after the operation. Moreover, they observed that digital systems allowed to precisely evaluate the point of air leak resolution and that the entity of pleural pressure is directly correlated with the size of the postoperative residual pleural space (21).
Cafarotti et al. reported a single-center series of 55 consecutive outpatient video-assisted thoracoscopic (VAT) wedge resections for pulmonary lesions and interstitial disease; pleural drainage management was based on a digital chest drainage system; the Authors concluded that pleural drainage can be safely removed two hours after VATS, thanks to the digital system; they report that outpatient VAT wedge resections managed with a digital system had both low complication rates as well as led to fewer re-admissions (22).
De Waele et al. recently reported the results of a prospective randomized trial comparing total volume of postoperative fluid drainage, the duration of pleural drainage in situ, prolonged air-leak incidence, total length of stay and the correlation between pleural effusion and entity of inflammation in two arms (digital drainage system vs analogic drainage system): although they confirmed the benefits of the digital drainage in decreasing PALs—as previously reported—they did not demonstrate a decrease of pleural fluid amount by using the digital system (23).
Arai et al. reported the results of a single-center retrospective case control study showing the non-inferiority of the digital Thopaz system compared to a standard analogic system in terms of outcomes after surgery, including types of operation, period of chest tube placement, chest tube reinsertion rate and clamping test rate that did not differ significantly between the groups. The authors report a minor instability of uncertain cause of the digital device, presenting—however—equivalent performance to the standard drainage system in terms of postoperative chest tube management. Major reported advantages offered by the digital device were more objective data, an improvement of mobility for the patient due to its small dimensions and the easy and fast set up (24).
Shoji et al. enrolled 112 consecutive patients - undergoing pulmonary resection - and subsequently managed with digital drainage system; they then compared PALs rate, duration of pleural drainage and complications rate with a group of 121 consecutive patients previously managed with analogic drainage system after pulmonary resection, using propensity score matching. They observed that mean duration of chest drainage was significantly shorter with digital drainage system than analogic system, concluding that management of PALs with digital drainage appears to reduce the duration of chest tube after lung resection (25).
Cho et al. reported the results of a prospective randomized study on sixty patients comparing Wi-Fi (Wireless-Fidelity) digital chest drainage system with conventional underwater-seal chest bottle system: they concluded that digital system was effective on reducing the length of chest tube by real time monitoring, emphasizing good results even in terms of patients’ satisfaction assessed by questionnaire. On the contrary the Authors report some risks in management of emergency situation like disconnection or malfunction of the device, suggesting intermediate step before home discharge (26); in case of doubts of malfunctioning or accidental disconnection, we recommend to check air leak status by a Bulau bottle or a standard analogic system before proceeding with chest drain removal.
A case of combined use of a digital drainage system and endobronchial Watanabe spigot in a patient with persistent pneumothorax with multiple pulmonary metastases has been recently reported by Shiroyama et al. emphasizing that that real-time quantitative evaluation of air leak is useful for determining the efficacy of endobronchial Watanabe spigot and balloon test during bronchoscopic occlusion (17); moreover, patient’s movement and positions’ changes can modify the entity of the air leaks: for this reason the 24-h monitoring that the digital system offers may be useful to correctly determine the presence or absence of air leaks (27).
In this review we analyzed eight series reporting results on 1,718 enrolled patients disclosing a clear benefit from digital system in terms of duration of chest tube after lung resection for air leak; on the contrary, no benefit has been demonstrated in terms of total amount of pleural fluid collection.
Good results in terms of patients’ satisfaction—assessed by questionnaire—have been reported but some risks in management of emergency situation have been highlighted, suggesting intermediate step before home discharge.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was commissioned by the Guest Editors (Marco Anile, Daniele Diso) for the series “Management of Air Leaks After Thoracic Surgery” published in Journal of Xiangya Medicine. The article has undergone external peer review.
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.12.05). The series “Management of Air Leaks After Thoracic Surgery” was commissioned by the editorial office without any funding or sponsorship. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Petrella F, Rizzo S, Radice D, et al. Predicting prolonged air leak after standard pulmonary lobectomy: computed tomography assessment and risk factors stratification. Surgeon 2011;9:72-7. [Crossref] [PubMed]
- Cerfolio RJ, Bass CS, Pask AH, et al. Predictors and treatment of persistent air leaks. Ann Thorac Surg 2002;73:1727-30; discussion 1730-1.
- Varela G, Jiménez MF, Novoa N, et al. Estimating hospital costs attributable to prolonged air leak in pulmonary lobectomy. Eur J Cardiothorac Surg 2005;27:329-33. [Crossref] [PubMed]
- Brunelli A, Xiume F, Al Refai M, et al. Air leaks after lobectomy increase the risk of empyema but not of cardiopulmonary complications: a case-matched analysis. Chest 2006;130:1150-6. [Crossref] [PubMed]
- Venuta F, Rendina EA, De Giacomo T, et al. Technique to reduce air leaks after pulmonary lobectomy. Eur J Cardiothorac Surg 1998;13:361-4. [Crossref] [PubMed]
- Varela G, Jiménez MF, Novoa NM, et al. Postoperative chest tube management: measuring air leak using an electronic device decreases variability in the clinical practice. Eur J Cardiothorac Surg 2009;35:28-31. [Crossref] [PubMed]
- Filosso PL, Nigra VA, Lanza G, et al. Digital versus traditional air leak evaluation after elective pulmonary resection: a prospective and comparative mono-institutional study J Thorac Dis 2015;7:1719-24. [PubMed]
- Cerfolio RJ, Bryant AS. The benefits of continuous and digital air leak assessment after elective pulmonary resection: a prospective study. Ann Thorac Surg 2008;86:396-401. [Crossref] [PubMed]
- Bertolaccini L, Rizzardi G, Filice MJ, et al. ‘Six sigma approach’ - an objective strategy in digital assessment of postoperative air leaks: a prospective randomised study. Eur J Cardiothorac Surg 2011;39:e128-32. [Crossref] [PubMed]
- Brunelli A, Salati M, Refai M, et al. Evaluation of a new chest tube removal protocol using digital air leak monitoring after lobectomy: a prospective randomized trial. Eur J Cardiothorac Surg 2010;37:56-60. [Crossref] [PubMed]
- Filosso PL, Ruffini E, Solidoro P, et al. Digital air leak monitoring after lobectomy for primary lung cancer in patients with moderate COPD: can a fast-tracking algorithm reduce postoperative costs and complications? J Cardiovasc Surg (Torino) 2010;51:429-33. [PubMed]
- Pompili C, Detterbeck F, Papagiannopoulos K, et al. Multicenter international randomized comparison of objective and subjective outcomes between electronic and traditional chest drainage systems. Ann Thorac Surg 2014;98:490-6; discussion 496-7. [Crossref] [PubMed]
- Lijkendijk M, Licht PB, Neckelmann K. Electronic versus traditional chest tube drainage following lobectomy: a randomized trial. Eur J Cardiothorac Surg 2015;48:893-8; discussion 898. [Crossref] [PubMed]
- Miller DL, Helms GA, Mayfield WR. Digital Drainage System Reduces Hospitalization After Video-Assisted Thoracoscopic Surgery Lung Resection. Ann Thorac Surg 2016;102:955-61. [Crossref] [PubMed]
- Cerfolio RJ, Varela G, Brunelli A. Digital and smart chest drainage systems to monitor air leaks: the birth of a new era? Thorac Surg Clin 2010;20:413-20. [Crossref] [PubMed]
- Thopaz Digital Chest Drainage System. Last accessed on September 19th, 2017. Available online: https://www.medela.com/healthcare/products/cardiothoracic-drainage/thopaz
- Borri A, Leo F, Veronesi G, et al. Extended pneumonectomy for non-small cell lung cancer: Morbidity, mortality, and long-term results. J Thorac Cardiovasc Surg 2007;134:1266-72. [Crossref] [PubMed]
- Spaggiari L, Galetta D, Veronesi G, et al. Superior vena cava replacement for lung cancer using a heterologous (bovine) prosthesis: Preliminary results. J Thorac Cardiovasc Surg 2006;131:490-1. [Crossref] [PubMed]
- Coughlin SM, Emmerton-Coughlin HM, Malthaner R. Management of chest tube after pulmonary resection: a systematic review and metaanalysis. Can J Surg 2012;55:264-70. [Crossref] [PubMed]
- Leo F, Duranti L, Girelli L, et al. Does external pleural suction reduce prolonged air leak after lung resection? Results from the AirINTrial after 500 randomized cases. Ann Thorac Surg 2013;96:1234-9. [Crossref] [PubMed]
- Takamochi K, Imashimizu K, Fukui M, et al. Utility of Objective Chest Tube Management After Pulmonary Resection Using a Digital Drainage System. Ann Thorac Surg 2017;104:275-83. [Crossref] [PubMed]
- Cafarotti S, Cusumano G, Giuliani M, et al. Extra-anatomical VATS lung resection: the outpatient experience with the aid of a digital chest drain device. Eur Rev Med Pharmacol Sci 2015;19:3850-4. [PubMed]
- De Waele M, Agzarian J, Hanna WC, et al. Does the usage of digital chest drainage systems reduce pleural inflammation and volume of pleural effusion following oncologic pulmonary resection?-A prospective randomized trial. J Thorac Dis 2017;9:1598-606. [Crossref] [PubMed]
- Arai H, Tajiri M, Kameda Y, et al. Evaluation of a digital drainage system (Thopaz) in over 250 cases at a single site: A retrospective case-control study. Clin Respir J 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Shoji F, Takamori S, Akamine T, et al. Clinical Evaluation and Outcomes of Digital Chest Drainage after Lung Resection. Ann Thorac Cardiovasc Surg 2016;22:354-8. [Crossref] [PubMed]
- Cho HM, Hong YJ, Byun CS, et al. The usefulness of Wi-Fi based digital chest drainage system in the post-operative care of pneumothorax. J Thorac Dis 2016;8:396-402. [Crossref] [PubMed]
- Shiroyama T, Okamoto N, Tamiya M, et al. Effective Management of Persistent Pneumothorax Using a Thopaz Digital Drainage System Combined with an Endobronchial Watanabe Spigot. Intern Med 2016;55:663-5. [PubMed]
Cite this article as: Petrella F, Borri A, Spaggiari L. Management of air leaks after thoracic surgery: old style or digital drainage? J Xiangya Med 2018;3:2.