
Hypothenar Hammer syndrome: importance of MR and conventional angiographic findings
Introduction
Hypothenar Hammer Syndrome (HHS) is a rare diagnosis of ulnar artery insufficiency caused by repetitive blunt trauma to the hypothenar region of the hand. First coined by Conn et al. in 1970, HHS is most prevalent among middle-aged men with occupations that result in the frequent use of the hypothenar region of the hand to pound or squeeze hard objects, examples of which include construction workers, auto mechanics, and miners (1). There have also been incidences of HHS associated with overexposure to the use of vibratory tools and machinery, as well as in athletes from sports where trauma to the palm frequently occurs (2). Patients may present with unilateral Raynaud’s phenomenon, tenderness to the hypothenar region, pain and discoloration of the digits, most commonly the 4th and 5th digits, and increased sensitivity to cold in the affected hand. Symptoms are usually episodic, and may or may not be precipitated immediately by trauma. In severe cases, ulceration and necrosis can result in gangrene of the digits (3). In primary care settings where HHS may be misdiagnosed as musculoskeletal overuse, increase awareness can lead to early intervention before ischemic changes become irreversible (4). In this case report, we highlight the imaging findings associated with HHS using angiography and diagnostic features that can distinguish HHS from other diseases with similar symptomatology.
Case presentation
The patient is a 46-year-old right-hand dominant male who works in auto upholstery presented to his primary care provider with a complaint of progressive left-hand pain and numbness. His symptoms involve the ulnar aspect of his hand, in particular, the left 4th and 5th digits, progressively worsening for the past 3 years. The patient states that he is regularly exposed to repetitive trauma to his palm regions. He was previously diagnosed with right-hand HHS, which was treated surgically with resection of a pseudoaneurysm and primary repair of the ulnar artery. The left-hand pain is not particularly relieved by any medications but was aggravated after a more recent trauma to his left wrist. He has a history of tobacco use, approximately 1 pack per week but quit 3 years prior to presentation. He is otherwise in a good state of health.
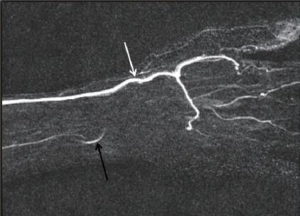
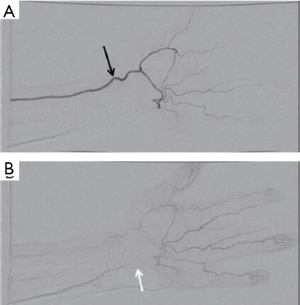
During his evaluation in the primary care physician’s office, the patient was found to have palpable ulnar and median pulses, slightly diminished on the left. The Allen test is positive. Electromyography performed demonstrated normal conduction of the left ulnar and median nerves. At this time, the patient was referred to our imaging center for magnetic resonance angiography (MRA) due to high clinical suspicion for HHS. On MRA, the patient is found to have occluded left ulnar artery in the region of the ulnar canal, also known as Guyon’s canal (Figure 1). There was no corkscrew of the distal digital arteries. There was no evidence of fracture of the carpal bones. Subsequently, the patient was referred to angiography of the left upper extremity, which demonstrated progressive narrowing and delayed opacification of the left ulnar artery with occlusion at the level of the carpal bones (Figure 2). Imaging findings were consistent with the HHS.
The patient was subsequently referred to a hand surgical specialist due to progressive symptoms. The patient was subsequently taken to the operating room for a reverse saphenous vein graft to bypass the thrombosed left ulnar artery. Intraoperatively, an occluded segment of the ulnar artery was noted in the Guyon’s canal, noted to have some intimal disease. The patient tolerated the procedure well, with a good ulnar pulse.
Discussion
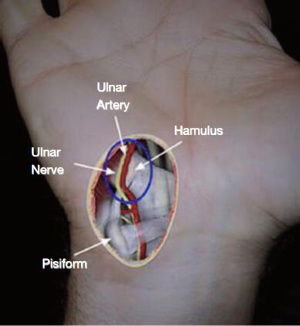
The ulnar artery branches off at the level of Guyon’s Canal, with one branch forming the deep palmar arch while the other branch continues to exit Guyon’s canal to form the superficial palmar arch, both with radial artery contributions (Figure 3). Study of arterial pattern estimates that in 37% of individuals, the superficial palmar arch is derived solely from the ulnar artery (5). The course of the artery just anterior to the hamate bone coupled with the thin overlaying tissue makes this portion of arterial supply susceptible to injury. Repetitive trauma to this region compresses the ulnar artery against the underlying bone (hamate), resulting in intimal deterioration that encourages the formation of an aneurysm, thrombotic occlusion, and vasospasm (6). Similar mechanisms have been described in several other vascular disease patterns (7). Due to the proximity of the ulnar artery to the ulnar nerve, associated compression of the nerve either from the trauma or by aneurysm growth can cause additional symptoms such as paresthesia of the digits (8).
Diagnosis of HHS can be made with Allen test, Doppler ultrasound, and angiography. When performing Allen test, a patient’s radial and ulnar arteries are compressed simultaneously to reduce blood flow to the hand. The pressure is released to one artery at a time to measure the time it takes for the color to return to the palm. A refill time of less than 5 secs is normal, negative for Allen’s test. A positive Allen’s test in HHS is characterized by normal filling by the radial artery and delayed filling by the ulnar artery, suggesting occlusion to blood flow. The sensitivity of the Allen test for HHS is 83% (2). However, a positive Allen’s test can be found in wide variety of conditions such as incomplete anastomosis between the radial and ulnar artery branches. While Allen’s test is easy to implement in a clinic setting, it lacks specificity and should be used in conjunction with other diagnostic tools.
Another diagnostic tool often used to study peripheral vasculature is Doppler ultrasound. This non-invasive procedure has been used in previous cases to assess thrombosis and aneurysmal dilatation to the ulnar artery (9). However, the gold standard and deterministic tool used in the diagnosis of HHS remain to be the conventional angiography. Features of HHS on angiography include the tortuosity, corkscrew-like appearance of the ulnar artery at the hypothenar eminence, aneurysmal dilation, occlusion, or stenosis in the same region that interrupts blood flow to the palmar arches (3). Computed tomography angiography (CTA) and MRA have also been used with the added benefits of being able to detect bony deformities and traumatic lesions, both being minimally invasive (10). The downside of using CTA and MRA to study ulnar patency is the inability to provide quantitative information on blood flow.
While the diagnosis of HHS is characterized by ulnar insufficiency, abnormalities in ulnar artery flow associated with trauma appear to be more common and can often remain asymptomatic. Ginn et al. studied the prevalence of ulnar artery abnormalities and ischemic changes to the digits in baseball players (11). Result suggests that catchers are more likely than other players to experience early vascular and ischemic changes to the ulnar artery despite having no report of symptoms, which is significant because catchers experience higher incidences of hand trauma from catching high-speed impact balls. Such observation is not unique to baseball. However, it is interesting to note not all individuals with a history of hypothenar trauma are diagnosed with HHS. A cohort study on 79 auto-mechanics who habitually use the hypothenar region of their hands revealed an HHS incidence of 14% (12). Another study of 300 individuals with occupational exposure to vibratory machinery found an HHS incidence of 9% (2). Histological examination of resected ulnar arteries from patients diagnosed with HHS suggests a higher incidence of vascular changes similar to fibromuscular dysplasia, which suggests an anatomical susceptibility that may predispose certain individual to HHS, which could explain the low incidence among at risk population (13). Additionally, there is also evidence showing a positive correlation with tobacco use in HHS patients (14).
The clinical presentation Raynaud’s phenomenon and digital ischemia may result in misdiagnosing HHS for diseases with similar symptomatology and of higher prevalence. Differential diagnosis includes primary Raynaud’s syndrome, connective tissue disorders, vasculitis, emboli stemming from large vessel disease, thromboangiitis obliterans (Buerger’s Disease), and coagulation disorders (3). Primary Raynaud’s is characterized by vasospasm in the digits leading to pain, discoloration, and cold intolerance in absence of underlying etiology. A form of reversible Raynaud’s has been linked to exposure to vibratory tools, much like in the case with HHS, named hand-arm vibration syndrome (HAVS) (15). Their shared etiology linked to occupational overuse makes distinguishing the two syndromes difficult but important in clinical management. Unlike HHS, abnormal angiographic findings of primary Raynaud’s and HAVS are typically limited to distal digital arteries, with reports of cork-screw appearances of collaterals (16,17). The digital discoloration associated with HHS also differs from the triphasic pattern of white-blue-red observed in Raynaud’s. In a majority of HHS cases, symptoms occur only in the dominant hand, sometimes in both hands in 7% of cases (14). Therefore, bilateral involvement would suggest other causes. In addition, as HHS is linked to trauma from overuse of the hands, lower extremity symptoms are very unlikely, which are commonly seen in connective tissue disorders, vasculitis, and Buerger’s. This entity should be kept in mind when a cardiac patient with certain occupational hazards has to undergo radial artery access for catheterization.
Treatment modalities for HHS focus on prevention of further trauma and restoration of ulnar arterial flow and range from percutaneous thrombin injection for ulnar artery aneurysm, which has similar success as for visceral arterial thrombin injection to surgical management with venous grafts (18). Due to the rarity of HHS diagnosis, there has yet to be sufficient evidence for a standard of care to be established. Conservative options include avoiding trauma to the hypothenar region which may require additional protection or change of occupation, smoke cessation, prescription of vasodilators, calcium-channel blockers, and antiplatelet therapy (9). Avoiding cold exposure is also recommended to minimize vasospasms and sympathetic aggravation. Surgical intervention may be indicated in addition to conservative management in severe cases for aneurysm repair and thrombi removal. Long-term follow-up of 12 patients who received vascular reconstruction following diagnosed with HHS showed persistent ulnar patency after in 75% of patients after 4.5 years with overall improvement of symptoms (19). The success of treatment will depend on the severity of ischemia, as well as the type of intervention and surgical procedure used. Until larger, prospective studies can take place to compare the efficacies of inventions, treatment of HHS will continue to vary case-by-case.
Conclusions
Clinical presentation of HHS includes Raynaud’s phenomenon, pain, and tenderness to the digits and hypothenar region, and increased cold sensitivity. Especially at risk of developing HHS are individuals with a history of repetitive trauma to the hypothenar region of the palm, either occupational or recreational. Patients who present with these symptoms, along with a history working in but not limited to construction, auto repair, mining, carpentry, as well as those of athletic background, should be evaluated for the diagnosis of HHS. The gold standard diagnostic test is angiography which can confirm ulnar insufficiency due to aneurysmal dilation or thrombi formation. Clinical examination, angiographic findings, and patient history can distinguish HHS from other diseases with symptomatology. Correct diagnosis can ensure to proper and timely therapeutic response that can lead to improvement of symptoms and reverse ischemic changes. Although larger multicenter studies will be needed to determine the best treatment course, surgical interventions have been shown to have good outcomes in restoring patency to the ulnar artery. This entity should be kept in mind when a cardiac patient with certain occupational hazards has to undergo radial artery access for catheterization. Additionally, patients at risk of developing HHS given their background and history of tobacco use should be educated in primary care settings to improve hand protection and minimize preventable trauma.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.10.01). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Conn J Jr, Bergan JJ, Bell JL. Hand ischemia: hypothenar hammer syndrome. Proc Inst Med Chic 1970;28:83. [PubMed]
- Kaji H, Honma H, Usui M, et al. Hypothenar hammer syndrome in workers occupationally exposed to vibrating tools. J Hand Surg Br 1993;18:761-6. [Crossref] [PubMed]
- Ablett CT, Hackett LA. Hypothenar hammer syndrome: case reports and brief review. Clin Med Res 2008;6:3-8. [Crossref] [PubMed]
- Gardiner GA, Tan A. Repetitive Blunt Trauma and Arterial Injury in the Hand. Cardiovasc Intervent Radiol 2017; [Epub ahead of print]. [Crossref] [PubMed]
- Coleman SS, Anson BJ. Arterial patterns in the hand based upon a study of 650 specimens. Surg Gynecol Obstet 1961;113:409-24. [PubMed]
- Kumar Y, Hooda K, Lo L, et al. Ulnar artery aneurysm and hypothenar hammer syndrome. BMJ Case Rep 2015;2015:bcr2015211444.
- Li S, King BN, Velasco N, et al. Cystic adventitial disease-case series and review of literature. Ann Transl Med 2017;5:327. [Crossref] [PubMed]
- Monacelli G, Rizzo MI, Spagnoli AM, et al. Ulnar artery thrombosis and nerve entrapment at Guyon's canal: our diagnostic and therapeutic algorithm. In Vivo 2010;24:779-82. [PubMed]
- Coulier B, Goffin D, Malbecq S, et al. Colour duplex sonographic and multislice spiral CT angiographic diagnosis of ulnar artery aneurysm in hypothenar hammer syndrome. JBR-BTR 2003;86:211-4. [PubMed]
- Hui-Chou HG, McClinton MA. Current options for treatment of hypothenar hammer syndrome. Hand Clin 2015;31:53-62. [Crossref] [PubMed]
- Ginn TA, Smith AM, Snyder JR, et al. Vascular changes of the hand in professional baseball players with emphasis on digital ischemia in catchers. J Bone Joint Surg Am 2005;87:1464-9. [PubMed]
- Little JM, Ferguson DA. The incidence of the hypothenar hammer syndrome. Arch Surg 1972;105:684-85. [Crossref] [PubMed]
- Ferris BL, Taylor LM Jr, Oyama K, et al. Hypothenar hammer syndrome: proposed etiology. J Vasc Surg 2000;31:104-13. [Crossref] [PubMed]
- Scharnbacher J, Claus M, Reichert J, et al. Hypothenar hammer syndrome: a multicenter case-control study. Am J Ind Med 2013;56:1352-8. [PubMed]
- Cooke RA. Hypothenar hammer syndrome: a discrete syndrome to be distinguished from hand-arm vibration syndrome. Occup Med (Lond) 2003;53:320-4. [Crossref] [PubMed]
- Cooke R, Sadhra S. Vascular hand-arm vibration syndrome-magnetic resonance angiography. Occup Med (Lond) 2016;66:756. [Crossref] [PubMed]
- Fujii Y, Teragawa H, Kihara Y, et al. Corkscrew collaterals in Raynaud's syndrome. BMJ Case Rep 2016;2016:bcr2016215841.
- Chauhan U, Puri SK, Jain N, et al. Percutaneous thrombin injection under sonographic guidance for exclusion of non-catheterizable post-pancreatitis pseudoaneurysm of the superior mesenteric artery: a minimally invasive and expeditious treatment option. J Med Ultrason (2001) 2016;43:295-9. [PubMed]
- Kitzinger HB. Hypothenar Hammer Syndrome: Long-Term Results After Vascular Reconstruction. Ann Plast Surg 2016;76:40-5. [Crossref] [PubMed]
Cite this article as: Geng M, Singh T. Hypothenar Hammer syndrome: importance of MR and conventional angiographic findings. J Xiangya Med 2017;2:70.


