Permanent cardiac pacing activities in a tertiary sub-Saharan centre
Introduction
Permanent Pace makers are implanted to prevent or treat bradycardia causes by disorders of the cardiac conduction system. In sub-Saharan countries except South Africa, cardiac pacing activity is poorly developed due to shortage of qualified personnel and lack of appropriate infrastructures (1). The Cardiac centre Shisong inaugurated in 2009 is a well-equipped with ultra-modern technologies institution offering a wide range of non-invasive, invasive procedures and open-heart surgery with extracorporeal circulation (2). The objective of the study is to report the cardiac pacing activities of the centre, the follow-up of implanted cases and challenges encountered from the 10th November 2009 till the 10th March 2016.
Methods
Following patient referral the clinical indication for pacemaker therapy was established from the history and the diagnosis confirmed with a 12 lead electrocardiogram and the 24-hour Holter if necessary (3). Cardiac function was assessed with a transthoracic echocardiogram.
Pacemaker implantation was performed in the catheterization laboratory of the cardiac centre equipped with a fluoroscopic C arm. The implantation team was composed of an electrophysiologist who performs the procedure, assisted by a scrub nurse, a circulating nurse helping in checking the intraoperative parameters, and a radiologist technician operating the fluoroscope for imaging. Monitored parameters were the heart rhythm, the heart rate, non-invasive blood pressure and peripheral oxygen saturation.
A standard subclavian approach (4) was used after infiltration with local anesthesia with Lidocaine. In all cases antibiotics were continued for 6 more days. The left side was the most used. The right side was used in case of anatomical abnormalities of vessels on the left side. After puncture of the vein, a guidewire was sent. The introducer was then inserted follow by the leads, first ventricular and later auricular. In case of resynchronization therapy, the coronary sinus lead was inserted in the targeted vein. Prior to the leads fixation, the r wave, p wave, r’ wave and pacing thresholds were checked. Target values were R wave greater than 9 millivolts, P wave greater than 2 millivolts, lead impedance less than 1,000 Ohms and pacing thresholds less than 1 Volt. Diaphragmatic pacing as checked at 10 Volts. The device leads were connected to the pulse generator and the wound closed in layers after good hemostasis. An arm sling was used in all cases to restrict the movement of the arm on the operation side and the patient was transferred to the ward.
Patients were monitored in the ward for 24 hours to prevent lead displacement. The day after the implant the device was checked. Seven day after implantation, patients were discharged, were given both the device implantation and device check reports. Patients were adviced to maintain the arm sling for two weeks and come back for follow up after three months. Pacemakers checks and complications management were done mainly by the electrophysiologist. Informed consent was obtained from each patient and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee. This is a descriptive study; results are presented as the mean ± the standard deviation. All statistical analyses were performed using the SPSS 11 program; for statistical difference the Student t-test and P<0.05 was considered significant.
Patients
From the 10th November 2010 till 10th March 2016, 130 patients underwent a device implantation in the cardiac centre Shisong. The permission to conduct the study was given by the Ethics committee of the Cardiac Centre. Data extracted from the records of implanted patients were demographics, clinical indications for device implantation, the electrocardiogram, the echocardiogram.
Results
A hundred and thirty patients benefited from a device in the institution, 52 were female and 78 were male with a mean age of 62.2±17 years old. The clinical characteristic of patients is listed in Table 1.
Table 1
| Item | Value |
|---|---|
| Total number of patients | 130 |
| Age at diagnosis (years) | 62.2±17 |
| Symptoms | |
| Dizziness | 85 |
| Shortness of breath | 91 |
| Fatigue | 79 |
| Adam stokes attack | 10 |
| Palpitation | 61 |
| No symptoms | 6 |
| Comorbidity | |
| Hypertension | 102 |
| Arthrosis | 52 |
| Diabetes mellitus | 25 |
Bradypacing
In the Cardiac Centre Shisong, for bradypacing were implanted 124 pace makers. Ten patients having atrial fibrillation with low ventricular response benefited from a single chambered pace maker. Sick sinus node was diagnosed in 36 patients; 32 cases benefited from a dual chambered pace maker and 4 from a single chambered pace maker. Seventy-eight cases had completed atrioventricular block and were implanted 5 patients single chambered and 73 dual chambered pace makers. In this group with 5 children, 3 had sick sinus disease and 2 had post-surgical complete atrioventricular block. In patients with heart rate less than 35 b/min, for a safe and smooth procedure, a temporal pace maker was inserted and removed immediately after connection of the leads to the device.
Tachypacing
Four intracardiac cardioverter defibrillators were implanted in 4 males, 3 single chamber and 1 double chamber. Three patients were at high risk presenting with hypertrophic cardiomyopathy and one was secondary prophylaxis of sudden death in a case with dilated cardiomyopathy with very poor left ventricular systolic function.
Cardiac resynchronization therapy
This therapy was performed in two ladies fulfilling the criteria: congestive heart failure group III–IV NYHA, left ventricle diastolic diameter more the 65 mm, ejection fraction less than 35% and complete left bundle branch block on the electrocardiogram.
All devices implanted were from the same company. All the ventricular leads were with passive fixation meanwhile the atrial leads were screw-in.
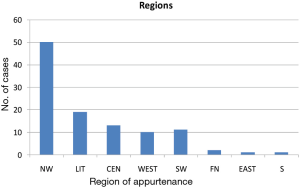
Some patients were coming from neighboring countries: a patient from Nigeria, a patient from Democratic republic Congo, a patient from Tchad. The rest was coming from the different regions of Cameroon, the North West region being the first in number of implanted patients (Figure 1).
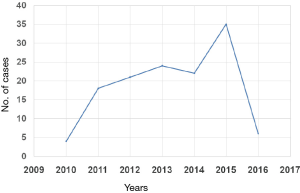
The pacing activities of the cardiac Centre Shisong got a peak in 2015 with 36 implanted devices (Figure 2).
Comorbidities
The comorbidities were: hypertension, diabetes mellitus type 2, peptic ulcer disease, polyarthritis and arthrosis.
Parameters
The intra-operative parameters were acceptable and listed in Table 2.
Table 2
| Parameters | Value |
|---|---|
| Threshold (V) at 0.4 ms | |
| Atrial | 0.9±0.2 |
| Ventricular | 0.6±0.4 |
| Impedance (Ohm) | |
| Atrial lead | 643±1.2 |
| Ventricular lead | 612±1.4 |
| P wave sensing (mV) | 1.9±0.7 |
| R wave sensing (mV) | 9±0.4 |
Complications of the procedure
Complications (Table 3) were seen postoperatively and during the follow-up: 4 cases with pocket infection, 4 leads displacements. Pneumothorax was diagnosed in 2 patients—they benefited from tap with very good outcome. Hematoma was seen in 2 patients post operatively the second day after the procedure due to agitation.
Table 3
| Complications | Number |
|---|---|
| Pocket infection | 4 |
| Lead displacement | 4 |
| Pneumothorax | 2 |
| Hematoma | 2 |
Follow-up
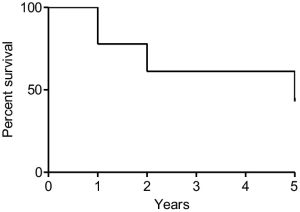
During the follow up period, three patients died in the acute post implantation period, and we registered 7 more deaths after 5 years. The Kaplan-Meyer curve is presented in Figure 3. The causes of death were: chronical renal failure, stroke, traffic road accident.
Discussion
We see that symptoms before implantation are the same as in the study of Ondze K et al who reported asthenia, dyspnoea, and syncope being the main ones (5). In our study, the majority of implants was performed in male, the mean age of patients at implantation being the same like the date reported in the study of Tamatey Martin et al (6). In Congo patients were older with a mean age of 70.4±6 years old (5). The difference in age should probably due to the fact that in the study were included children with sick sinus node and post-surgical complete atrioventricular block.
It was reported that in 3,580 European centres, a total of 500,411 pacemakers were implanted in 2013. The authors continue saying that excluding San Marino, the country with the highest density of implanting facilities was Germany (12.4 per million in habitants) and those with the lowest density were Egypt, Moldova, and Morocco with only 0.3 implantations per million inhabitants. In 2013, the mean PM implantation rate in the participating European society of cardiology countries was 532 pace makers units per million inhabitants. The implantation rate was highest in Belgium [1,218] and Germany [1,152], and lowest in Azerbaijan [14] and Egypt [30] (7). In Sub-Saharan Africa except South Africa (8), the implantation rate per million inhabitants is poorly determined; in the experience of Thomas et al. from Lagos (9), 100 patients were implanted between 1999 and 2004, without complications. In Enugu (10), 23 implants were done between 2001 and 2006. In Dakar (11), Senegal, 92 pacemakers were implanted over three years, 53% being reused recycled pace makers with the following complications: pocket infection in 5 patients, 3 leads displacement, 1 pace maker syndrome and 8 non pace maker related deaths. In Tunisia (12), in a study conducted by Hatem Bouaroui, 234 pacemakers were implanted in 23 years. We have more devices implanted in our study. The reduced number of cases in our countries generally is due to mainly to financial limitations, the appropriate infrastructure and qualified human resource present very limited. It is worth to mention that in Cameroon we were the first to implant double chambered pace makers.
In our study, there was no procedure-related death, neither perioperative mortality meaning that the procedure is safe.
In Congo the preference was given to the cephalic access instead of the subclavian as the study of Falase in Nigeria (13) and Bouaroui et al. (12) in Tunisia. This is a preference and school diversity. It was really surprising to see that implantation site in the Tunisian experience is the right side.
In some cases, complete atrioventricular block was post-surgical, reported also in the study of Edwin et al. In their study done in Ghana, six patients out of 242 had post-surgical complete atrioventricular block and benefited from doubled single chambered pace makers (14). Adeoye et al. in Ibadan (15) as in our case reported that the common indication foe the implant was severe bradycardia due to complete atrioventricular block. The most common cause of this disorder is not known in a greater number of patients. He continued reporting that the possible mechanisms are myocardial sclerosis, however it was strongly associated in a case with chronic chloroquine usage.
Some authors from Nigeria reported that most of the patients with complete atrioventricular block had single chambered pace makers and were doing well despite the fact that dual chambered pace makers are the best in this kind of pathology because they maintain the synchrony between the atria and ventricles (16). In our study, the majority of patients benefited from a dual chambered pace maker functioning in DDD mode. In Senegal, Tunisia, Singapore (17) and Nigeria, the commonest implantation was single chambered pace makers surely due to financial limitations.
In some patients having idioventricular rhythm, due to severe bradycardia and mainly to pace maker dependence during the check of intraoperative parameters, a temporal pacemaker was inserted for a smooth going of the procedure.
Complications of the procedure are known, reported and managed in the same way by Senegalese and Tunisian colleagues in almost the same percentages.
The follow-up in a setting with limited economic resources in very challenging, with death related to infectious and other non-communicable diseases.
In implanted cases the quality of life was better, the mortality lower than in non-implanted cases.
As far as ICD are concerned, excluding San Marino, Germany (336 per million inhabitants), the Czech Republic [301], and Belarus [292] had the highest implant rates while the lowest reported were in Algeria, Azerbaijan, and Morocco (1 per million inhabitants for each) (7). In Moldova no ICDs were implanted in 2013. In our experience 4 ICD were implanted in two years. In the past these patients were transferred to Europe for the procedure. We are still at the beginning of our activities and the future is really promising.
In Europe, a survey showed that the mean number of centres implanting pace makers per million inhabitants was 3.8 (7). There are currently three centres in Cameroon known to implant devices: Douala, Yaounde and Shisong for a population of 18 million inhabitants. In Nigeria with a population more than ten times the Cameroonian population, only 10 centres (13). Our governments and stakeholders should create and sustain well equipped tertiary centres for the invasive management of cardiovascular diseases; it will develop our countries and stop the brain and money drainage to western countries.
Besides eliminating risk of sudden death, reasons for an early PM implantation in patients with CAVB are prevention of morbidity, left ventricular dilatation and dysfunction and mitral regurgitation. Permanent pacemakers provide effective relief of symptoms and are life-saving in patients with symptomatic heart block. Since pacemakers are only implanted by cardiologists or cardiothoracic surgeons in tertiary hospitals, the rates of pacemaker implantation provide a readily auditable measure of tertiary health care (18). In developed countries patients with natural history of complete heart block are almost absent because of progress in medicine orientated in early detection and treatment of the conditions, meanwhile in developing countries with the lack of finances, infrastructures and human resources many cases are encountered (19).
In 2015 due to the sponsorship of the Archbishop Verdzekov Heart foundation more cases could be done. All patients presenting with financial limitations can benefit from the help of this foundation in the cardiac centre Shisong. The amount of money allocated to patients varies depending on the resources available and the screening of the level of poverty done by the officer in charge of the Foundation . All people are invited to contribute and participate to the activities of the foundation.
In sub-Saharan Africa, South Africa was the only country where intracardiac cardioverter defibrillators were implanted and bi-ventricular pacing was done. Fortunately in Cameroon and in central Africa for the very first time was implanted in 2013 the first intracardiac cardioverter defibrillator and later in 2015 bi-ventricular pacing was done. This manuscript is the first to officially document the implant of defibrillators and cardiac resynchronization therapy done in sub Saharan Africa in a different country than the Republic of South Africa.
Conclusions
Bradypacing, tachypacing and cardiac resynchronization therapy are procedures done in the cardiac Centre Shisong with good results and low complication rate. Our governments and stakeholders should create and sustain well equipped tertiary centres for the invasive management of cardiovascular diseases.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.07.06). The authors have no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. Informed consent was obtained from each patient and the study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki (as revised in 2013) as reflected in a priori approval by the institution’s human research committee.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Ikama SM, Makani J, Jouven X, et al. Permanent cardiac pacing: first Congolese experiment. Pan Afr Med J 2015;20:381. [Crossref] [PubMed]
- Budzee A, Tantchou Tchoumi JC, Ambassa JC, et al. The Cardiac Center of Shisong Hospital: the first cardio-surgical center in West and Central Africa is inaugurated in Cameroon. Pan Afr Med J 2010;4:4. [PubMed]
- Brignole M, Auricchio A, Baron-Esquivias G, et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the Task Force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Eur Heart J 2013;34:2281-329. [Crossref] [PubMed]
- Hess DS, Gertz EW, Morady F, et al. Permanent pacemaker implantation in the cardiac catheterization laboratory: the subclavian vein approach. Cathet Cardiovasc Diagn 1982;8:453-8. [Crossref] [PubMed]
- Ondze Kafata LI, Haggui A, Chomeni H, et al. La stimulation cardiaque au centre hospitalier universitaire de Brazzaville: champagne humanitaire d’implantation de pace makers. Rev Cames Sante 2014;2:63-8.
- Tamatey MN, Sereboe LA, Tettey MM, et al. Permanent pacemaker implantation in Accra. An 18 year review. Afr Ann Thorac Cardiovasc Surg 2012;7:47-50.
- Raatikainen MJ, Arnar DO, Zeppenfeld K, et al. Statistics on the use of cardiac electronic devices and electrophysiological procedures in the European Society of Cardiology countries: 2014 report from the European Heart Rhythm Association. Europace 2015;17:i1-75. [Crossref] [PubMed]
- Millar RNCardiac Arrhythmia Society of South Africa. 1998 survey of cardiac pacing in South Africa--report of the working group on registries of the cardiac arrhythmia society of South Africa (CASSA). S Afr Med J 2001;91:873-6. [PubMed]
- Thomas MO, Oke DA, Ogunleye EO, et al. Bradypacing: indications and management challenges in Nigeria. Pacing Clin Electrophysiol 2007;30:761-3. [Crossref] [PubMed]
- Ekpe EE, Aghaji MA, Edaigbini SA, et al. Cardiac pacemaker treatment of heart block in Enugu a 5-year review. Niger J Med 2008;17:7-12. [Crossref] [PubMed]
- Thiam M, Fall PD, Gning SB, et al. Cardiac pacing in West Africa: feasibility, problems, and perspectives. Ann Cardiol Angeiol (Paris) 2003;52:212-4. [Crossref] [PubMed]
- Bouraoui H, Trimech B, Chouchene S, et al. La stimulation cardiaque permanente: à propos de 234 patients. La tunisie Medicale 2011;89:604-9. [PubMed]
- Falase B, Sanusi M, Johnson A, et al. Analysis of a five years experience of permanent pace maker implantation at a Nigerian teaching Hospital: need for a national database. Pan Afr Med J 2013;16:16. [Crossref] [PubMed]
- Edwin F, Aniteye E, Tettey M, et al. Permanent complete heart block following surgical correction of congenital heart disease. Ghana Med J 2010;44:109-14. [PubMed]
- Adeoye PO, Okonta KE, Salam MA, et al. Experience with permanent pace maker insertion at the University College hospital, Ibadan, Nigeria Nigerian. Journal of Cardiology 2013;10:3-5.
- Thomas MO, Oke DA, Ogunleye EO, et al. Bradypacing: indications and management challenges in Nigeria. Pacing Clin Electrophysiol 2007;30:761-3. [Crossref] [PubMed]
- Teo WS, Kam RM. Pacemaker implantation in Singapore in 1997. Singapore Med J 1999;40:745-8. [PubMed]
- Zion MM, Marchand PE, Obel IW. Long-term prognosis after cardiac pacing in atrioventricular block. Br Heart J 1973;35:359-64. [Crossref] [PubMed]
- Tantchou Tchoumi JC, Foresti S, Lupo P, et al. Follow up in a developing country of patients with complete atrio-ventricular block. Cardiovasc J Afr 2012;23:538-40. [Crossref] [PubMed]
Cite this article as: Tantchou Tchoumi JC. Permanent cardiac pacing activities in a tertiary sub-Saharan centre. J Xiangya Med 2017;2:62.