A case of Churg-Strauss syndrome misdiagnosed as dermatitis
Introduction
Churg-Strauss syndrome (CSS) is a rare primary vasculitic disease as eosinophilic granulomatosis with polyangiitis (EGPA) that’s characterized by late-onset asthma, an eosinophilic vasculitis that affects the small and medium sized vessels (1). This syndrome was first described in 1951 by Jacob Churg and Lotte Strauss (2) and was initially called allergic angiitis and granulomatosis. Most CSS patients are adults in the third and fourth decades of life and there is a slight male predominance (2). Although a number of classification systems have been proposed, the American College of Rheumatology (ACR) proposed the following 6 classification criteria, and 4 out of 6 criteria should be present in the diagnosis of CSS: asthma, eosinophilia greater than 10%, paranasal sinusitis, pulmonary infiltration and no fixed, histological proof of vasculitis and mono- or poly-neuropathy. Using these criteria result in 85% sensitivity and 99.7% specificity to diagnose CSS (3). Here, we report a case of CSS that was confirmed by the ACR classification but was misdiagnosed as dermatitis initiate.
Case presentation
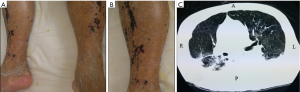
A 50-year-old male was admitted because of cough for more than 3 months and then the patient presented with night fever, cough, sputum, anorexia, pharyngalgia and a weight loss of 10 kg within the 3 months immediately prior to admission. But he had no night sweat, hemoptysis, headache and arthralgia. At that time, in the local hospital the eosinophil increased obviously in the peripheral blood and the lung CT (Figure 1) showed interstitial lesions and multiple scutellate vague in the lung of both sides, and the symptoms progressed rapidly. Based on the above clinical features, he was diagnosed as allergic pneumonia and received the antiallergic, corticosterone for topical use, anti-infectious, relieving cough and reducing sputum therapy. The systemic symptoms did not alter and even exacerbated. Therefore, he was admitted to our respiratory medicine department because of allergic pneumonia in June 14, 2013. He had been suffering from cerebral infarction for 2 months and denied history of allergic rhinitis.
When the respiratory symptoms appeared, macules, papules, scratch and hyperpigmentation could also be observed in the whole body, especially in the both lower limbs and the patient also complained of unbearable skin itchy. At that time, the patient visited the dermatological outpatient and the severe lesions were diagnosed as dermatitis, and the lesions showed slight improvement after receiving tropical corticosteroids therapy.
The physical examination revealed a moderate fever of 38.0 °C but the vital signs were stable. The skin examination revealed obvious macules, papules, scratch and hyperpigmentation on both extremities, and symmetry pitting edema could be examined in the both lower limbs, but no fester and pus (Figure 1). There were several enlarged lymph nodes touched in the both supraclavicular and infraclavicular fossaes, fossaes axillaris, iliac region. Light wheezing rale could be listened in the left lung. No other positive sign could be observed.
The laboratory findings showed an elevated white blood cell (WBC) count of 19.7×109/L (reference range, 4–10×109/L) with a differential count of neutrophils 54.4%, eosinophils 35.6%, an elevated absolute eosinophil count of 7.0×109/L (reference range, 0–0.5×109/L), an elevated creatinine level of 219.2 µmol/L (reference range, 53–132.6 µmol/L), an elevated lithic acid level of 783.5 µmol/L (reference range, 142–416 µmol/L), an elevated C-reactive protein (CRP) level of 29.90 mg/dL (reference range, 0–3 mg/dL), a declining immune globulin G level of 4.34 g/L and a declining immune globulin A level of 612.00 g/L. The prothrombin time (PT) was slightly prolonged to 13.1 seconds (reference range, 10.3–12.5 seconds), the activated partial thromboplastin time (APTT) was in the normal range of 28.7 seconds, the platelet count was in the normal range of 133×109/L. The patient was negative for twice examined P-ANCA, C-ANCA and antinuclear antibody. The erythrocyte sedimentation rate (ESR), C3, IgM, Tspot levels were within the normal ranges. The serology studies for hepatitis B and toxoplasmosis as well as for antibodies to HIV were negative and the VDRL was non-reactive.
The chest CT showed interstitial lesions and multiple scutellate vague in the lung of both sides. Pulmonary function test showed normal ventilation function but positive bronchial challenge test. The fibrolaryngoscope examination showed chronic sinusitis. Bone marrow hyperplasia, eosinophilia could be observed in the bone marrow aspiration.
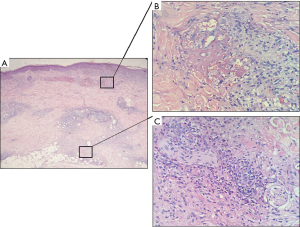
We performed hematoxylin-eosin staining on a section of a skin biopsy specimen from a hemorrhagic vesicle on the right lower leg. There was extensive vascular necrosis, and many histocytes, lymphocytes and eosinophils around the necrosis vessels in the upper dermis. Additionally, there were diffuse inflammatory cell infiltrations in the middle and lower dermis, and especially in the perivascular area. Many neutrophils, lymphocytes, neutrophil fragments and eosinophils were observed around the cutaneous vessels (Figure 2).
Discussion
CSS is a multisystem disease that’s characterized by asthma, peripheral eosinophilia, peripheral neuropathy, pulmonary infiltrates and paranasal sinus abnormalities. Its prevalence, in the general population, ranges from 0.5 to 2.7 cases/million inhabitants (4), and often observed in the patients in the third and fourth decades of their life.
Classical CSS can be divided into three clinical stages. Allergic rhinitis and asthma are typical symptoms in the first stage; Severe respiratory symptoms and severe eosinophilia in the peripheral blood are often observed in the second stage; in the third stage, CSS can affect virtually any organ system in the body and lead to the dysfunction of some important organs with poorer prognoses. However, our present patient had no allergy history and light respiration symptoms which may mislead the clinical doctor’s diagnosis. Skin lesions are important features of CSS, occur in about 55% of the cases (1,3) and often occur in the third stage which is the most severe clinical stage. The main types of skin lesions found in CSS include (I) erythematous maculopapules resembling erythema multiforme; (II) hemorrhagic lesions ranging from petechiae to extensive ecchymosis, and these lesions are often associated with wheals, necrosis and ulceration; (III) cutaneous and subcutaneous nodules that are usually deep-seated and tender with a predilection for the scalp. Our present patient had hardly any described lesions above, and he had only some common maculopapules but no ulceration and nodules which were often appeared in the vasculitis clinical cases. Meanwhile the severe scratch and escharosis was thought to be induced by factitial dermatitis so that ignoring the skin biopsy which was misdiagnose as dermatitis or drug rash initially. For the laboratory examine, some studies showed ANCA frequency in CSS to be just under 50% (5,6). Most often, EGPA patients’ ANCA have a perinuclear fluorescence-labeling pattern (P-ANCA), with anti-myeloperoxidase (MPO) specificity. Our present patient belongs to ANCA-negative patients, according with CSS studies before, which makes the diagnosis more difficult. Skin biopsy is helpful in the diagnosis and often occurs the typical microscopic performance. Typical pathology of CSS is extensive vascular necrosis, many eosinophils around the cutaneous vessels, and extravascular granuloma formation, and our pathology was completely consistent with the typical pathology performance.
The diagnosis of CSS should based on the following 6 classification criteria, and 4 out of 6 criteria should present in the diagnosis of CSS: asthma, eosinophilia greater than 10%, paranasal sinusitis, unfixed pulmonary infiltration and histological proof of vasculitis and mono- or poly-neuropathy. Our patient conformed 5 criteria except for mono- or poly-neuropathy. The differential diagnosis includes other vasculitis (e.g., microscopic polyarteritis, essential cryoglobulinemic vasculitis, Wegener’s granulomatosis), atopic dermatitis, drug reaction with eosinophilia and systemic symptoms(DRESS), hypereosinophilic syndrome (HES).
Most of CSS patients are sensitive to systemic corticosteroids which are a first-line therapy for CSS. Meanwhile, there are some alternative immunosuppressivedrugs such as cyclophosphamide, azathioprine and mycophenolate that have been used to treat the cases resistant to corticosteroids. Combination of corticosteroids and cyclophosphamide is the most efficient therapy of CSS. Intravenous immunoglobulin and plasmapheresis are also applied in the palliative therapy of CSS (7). Biological agents for treating cutaneous vasculitis is still under study. Inhibiting production of immune complex (Rituximab), inhibiting activation of inflammatory cells (Anti-Tumor Necrosis Factor α) and inhibiting chemotaxis of inflammatory cells (Anti-Human Relaxin or Interleukin-8) are the main research directions (8).
Patient outcome
A high dose of oral corticosteroid (prednisolone 1 mg/kg) for 10 days, human immune globulin (0.3 g/kg) for 7 days and some other symptomatic treatments such as anti-infectious, liver protection, nutrition support were used immediately at the time of diagnosis of CSS. However, the patient still aggravated after the therapy, and plasmapheresis was performed one time after the 7 days of diagnosis of CSS. While reduced peripheral three blood cell lines happened in 10 days after corticosteroid treating, and complicated sepsis and disseminated intravascular coagulation (DIC) induced by primary disease aggravation appeared. Finally the patient was dead in the 50 days of hospitalization in the Intensive Care Unit regretfully.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.07.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient’s daughter for publication of this manuscript and any accompanying images.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Lanham JG, Elkon KB, Pusey CD, et al. Systemic vasculitis with asthma and eosinophilia: a clinical approach to the Churg-Strauss syndrome. Medicine (Baltimore) 1984;63:65-81. [Crossref] [PubMed]
- Churg J, Strauss L. Allergic granulomatosis, allergic angiitis, and periarteritis nodosa. Am J Pathol 1951;27:277-301. [PubMed]
- Masi AT, Hunder GG, Lie JT, et al. The American College of Rheumatology 1990 criteria for the classification of Churg-Strauss syndrome (allergic granulomatosis and angiitis). Arthritis Rheum 1990;33:1094-100. [Crossref] [PubMed]
- González-Gay MA, García-Porrúa C. Systemic vasculitides. Best Pract Res Clin Rheumatol 2002;16:833-45. [Crossref] [PubMed]
- Sinico RA, Di Toma L, Maggiore U, et al. Prevalence and clinical significance of antineutrophil cytoplasmic antibodies in Churg-Strauss syndrome. Arthritis Rheum 2005;52:2926-35. [Crossref] [PubMed]
- Choi JH, Ahn IS, Lee HB, et al. A case of churg-strauss syndrome. Ann Dermatol 2009;21:213-6. [Crossref] [PubMed]
- Gayraud M, Guillevin L, le Toumelin P, et al. Long-term followup of polyarteritis nodosa, microscopic polyangiitis, and Churg-Strauss syndrome: analysis of four prospective trials including 278 patients. Arthritis Rheum 2001;44:666-75. [Crossref] [PubMed]
- Bolognia JL, JorizzoJL, Schaffer JV. Dermatology: 2-Volume Set, 3rd Edition. Elsevier (Singapore) Pte Ltd. and Peking University Medical Press. 2014.
Cite this article as: Wang B, Li J, Shi W. A case of Churg-Strauss syndrome misdiagnosed as dermatitis. J Xiangya Med 2017;2:57.