Phyllodes tumor of the breast—not all are self-detected
Introduction
The fibroepithelial neoplasm of the breast, classified as phyllodes tumor (PT), is a rare condition and its usual presentation is characterized by a self-detected lump, a rapidly growth tumor, and frequently large dimensions at the time of diagnosis (1,2). Average age at presentation is around 40 years old and mean tumor size is 4.3–8.3 cm (3-7). Percutaneous core-needle biopsy (CNB) has high positive and negative predictive values, but definitive diagnosis is determined with the study of the entire surgical specimen. Asymptomatic cases with PT are reported to be <10% (2,8), with the majority of tumors identify by medical physical examination or in breast imaging studies due other mammary symptoms. With increased breast awareness and breast cancer screening programs, smaller and incidental lesions are being found on imaging (4,9,10). The objective of this study was to describe the clinical, radiological, histopathologic, and therapeutic aspects of asymptomatic patients with PT of the breast, as well as to identify clinical differences between asymptomatic and symptomatic patients with PT in a sample of Mexican feminine population.
Methods
A retrospective cross-sectional study was conducted of consecutive patients with PT between August 2005 and August 2015, initiated after approval by the Institutional Review Board of Instituto de Enfermedades de la Mama and Fundación del Cáncer de Mama (IEM-FUCAM) in Mexico City. IEM-FUCAM is a high specialty and non-profit hospital that attends to open population of Mexico City and Metropolitan Area and has had a well-organized breast cancer screening program since 2000. Inclusion criteria included the following: female patients aged ≥16 years with a diagnosis of PT in breast tissue of CNB or in definitive surgical specimen. The variables studied included sociodemographic aspects, radiological characteristics, tumor features, and treatment. Radiological appearance of asymptomatic cases evaluates tumor margins, nodule density, echogenicity, lobulations, and vascularity. PT classification encompasses criteria adopted by the World Health Organization (WHO) Working Group (11), which evaluate mitoses, stromal hypercellularity, cellular pleomorphism, stromal pattern, margins, and heterologous elements and which divides tumors into benign, borderline, and malignant PT, including, for this purpose, only surgically treated cases. Data were obtained from the patients’ clinical, radiological files and from histopathological reports of their tumor tissues. Frequency distribution was evaluated with descriptive statistical techniques. Differences among continuous variables were tested, employing the Student t-test for normal distribution data or the Mann-Whitney U-test, and differences in the distribution of categorical variables were analyzed employing the Pearson chi-square test or Fisher exact test. All P values ≤0.05 were considered statistically significant, and all P values were two-sided. SPSS ver. 16.0 for Windows statistical software (SPSS, Inc.) was utilized for statistical analyses.
Results
General population
The IEM-FUCAM registered 346 PT in 344 patients during the 10-year period; 39 patients were excluded because they decided to treat at other hospitals. The present study included 305 patients (307 tumors) who were surgical treated at our Institute. Mean age was 41.7 years (range, 16–75 years), smoking were reported in 6.9%, systemic high blood pressure in 12.5%, and diabetes in 5.9%, mean body mass index (BMI) was 27.1 kg/m2 with 66.2% patients within the range of overweight or obesity. Premenopausal status predominated (77.7%), and age at menopause was 46.2 years in the 68 postmenopausal patients. Right and left breast were similar affected, and external quadrants were the most frequent localization (61.2%). Nearly all cases underwent preoperative biopsy: 281 (91.5%) tumors underwent a CNB in a physician’s office, and 21 (6.8%), ultrasound (US)-guided CNB. The five cases with excisional biopsy without preoperative biopsy were performed because US images were compatible with benign tumors in four patients and in one case with multifocal PT. Surgical procedures included 213 (69.8%) local wide excisions and 92 (30.2%) total mastectomies. Median tumor size in surgical specimen was 4.8 cm. Two mastectomies had multifocal disease.
Differences between asymptomatic and symptomatic patients
The most frequent condition comprised a self-detected palpable lump in 91.9% cases, with an average clinical tumor size of 4.5 cm and that was discovered 6 months previously. Asymptomatic patients were registered in 25 (8.1%) cases; these tumors were identified during periodic examination or through mammography or breast US studies, due to screening or mastalgia. During physical examination undergone by breast cancer specialists, nine (3%) cases were non-palpable mass, and in 15 (4.9%) patients, the tumors were not-well-identified due small tumor size, deep localization, or due to the large size of the mammary gland.
Asymptomatic patients presented some statistical differences compared with symptomatic patients (Table 1). Asymptomatic cases were 6 years older, had more pregnancies, had more breastfeeding, small mammographic tumor size, small US tumor size, small tumors in surgical specimen, and more conservative surgeries compared with symptomatic cases. Asymptomatic patients had other characteristics without statistically significant differences, such as more systemic high blood pressure cases, higher BMI, more postmenopausal women, and more benign PT. Due the nature of these study, conservative surgery were more in asymptomatic patients, compared to symptomatic patients (91.7% vs. 68%; P=0.005); the reason because two asymptomatic cases underwent mastectomy, was in one case the presence of multifocal PT and other case treated with mastectomy due ipsilateral breast cancer.
Table 1
| Variable | Symptomatic (n=282) | Asymptomatic (n=25) | P |
|---|---|---|---|
| Age† | 41.2±11.1 [16–75] | 47.6±10 [28–69] | 0.005 |
| Smoking | 20 (7.1%) | 1 (4%) | 0.584 |
| Systemic high blood pressure | 33 (11.7%) | 5 (20%) | 0.196 |
| Diabetes mellitus | 17 (6%) | 1 (4%) | 0.707 |
| BMI (kg/m2) | 26.9±5.4 | 28.7±5.5 | 0.130 |
| Age at menarche† | 12.7±1.6 | 13±1.4 | 0.327 |
| Age at first delivery† | 22.5±5.1 | 22.4±4.5 | 0.862 |
| Number of pregnancies | 2 [0–9] | 3 [1–10] | 0.013 |
| Breastfeeding (positive) | 172 (61%) | 20 (80%) | 0.042 |
| Use of hormonal contraceptives | 72 (25.5%) | 7 (28%) | 0.592 |
| Premenopausal | 222 (79%) | 15 (62.5%) | 0.062 |
| Postmenopausal | 59 (21%) | 9 (37.5%) | |
| Age at menopause† (n=68) | 46.4±6.7 | 45.1±4.1 | 0.276 |
| Right mammary gland affected | 142 (50.4%) | 12 (48%) | 0.658 |
| Tumor size‡ | |||
| US tumor size | 4 [1.2–32] | 2.6 [1.1–4] | <0.001 |
| Mammographic tumor size | 4.2 [1.2–25] | 2.1 [1–4] | <0.001 |
| Histopathologic biopsy report (n=302) | 280 | 22 | 0.001 |
| Fibrotic changes | 3 (1.1%) | 3 (13.6%) | |
| Fibroadenoma | 56 (20%) | 5 (22.7%) | |
| PASH | 6 (2.1%) | – | |
| Fibroepithelial neoplasia | 36 (12.9%) | 4 (18.2%) | |
| Phyllodes | 179 (63.9%) | 10 (45.5%) | |
| Surgical treatment | 0.005 | ||
| Wide excision (n=213) | 191 (68%) | 22 (91.7%) | |
| Mastectomy (n=92) | 90 (32%)§ | 2 (8.3%)¶ | |
| Phyllodes tumor subtype | 0.147 | ||
| Benign | 200 (70.9%) | 22 (88%) | |
| Borderline | 47 (16.7%) | 3 (12%) | |
| Malignant | 35 (12.4%) | 0 | |
| Pathologic tumor size‡ | 5 [1–30] | 3 [1.2–4.7] | <0.001 |
†, age in years; ‡, maximal tumor diameter in centimeters; §, one case of mastectomy with multifocal phyllodes tumor; ¶, one case of mastectomy with multifocal phyllodes tumor and other case treated with mastectomy due breast cancer. US, ultrasound; PASH, pseudoangiomatous stromal hyperplasia of the breast.
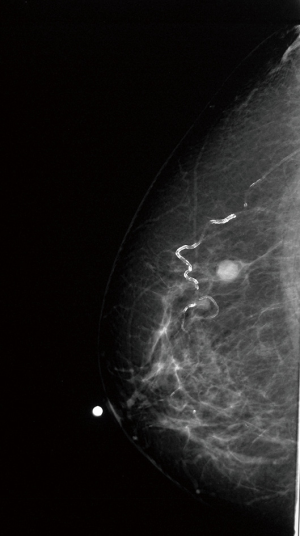
All patients had mammary image studies. In symptomatic cases, mammogram features of PTs appeared as a suspicious high density nodule in 100%, with lobular circumscribed margins in 90%, and according to the Breast Imaging-Reporting and Data System (BI-RADS) were classified as BI-RADS 4 in 90%; the US features were described as heterogeneous or mixed nodule in 86%, with macrolobular contours 80%, and with the presence of vascularity in 24%. The image characteristics in asymptomatic cases were different. Mammographic images showed a nodule without calcifications in 24 (96%) cases (Figure 1), and one (4%) case with focal asymmetry. The majority of nodules were isodense (75%) and well-circumscribed or with obscured margins. The BI-RADS 4 category was the most frequent qualification in mammographic studies (Table 2). The three cases with borderline PT had isodense nodules with obscured margins.
Table 2
| Variable | Total | Benign | Borderline |
|---|---|---|---|
| Mammogram and US | 25 (100%) | 22 | 3 |
| Radiologic findings | |||
| Nodule (M and US) | 24 (96%) | 21 | 3 |
| Asymmetry (M) and nodule (US) | 1 (4%) | 1 | – |
| Mammogram features of nodule (n=24) | |||
| Nodule density | |||
| Isodense | 18 (75%) | 17 | 3 |
| High density | 6 (25%) | 6 | – |
| Margins | |||
| Circumscribed | 12 (50%) | 12 | – |
| Obscured | 9 (37.5%) | 6 | 3 |
| Indistinct | 3 (12.5%) | 3 | – |
| BI-RADS, n=25 | |||
| 0 | 6 (24%) | 6 | – |
| 2 | 2 (8%) | 1 | 1 |
| 3 | 3 (12%) | 3 | 0 |
| 4 | 14 (56%) | 12 | 2 |
| US features of nodule, n=25 | |||
| Pattern | |||
| Hypo-echoic | 16 (64%) | 13 | 3 |
| Iso-echoic | 6 (24%) | 6 | – |
| Heterogeneous or mixed | 3 (12%) | 3 | – |
| Margins | |||
| Circumscribed | 18 (72%) | 15 | 3 |
| Obscured | 4 (16%) | 4 | – |
| Indistinct | 3 (12%) | 3 | – |
| Contour | |||
| Macrolobular | 20 (80%) | 17 | 3 |
| Microlobular | 4 (16%) | 4 | – |
| Angular | 1 (4%) | 1 | – |
| Vascularity (Doppler) | |||
| No vascularity | 22 (88%) | 20 | 2 |
| With vascularity | 3 (12%) | 2 | 1 |
| BI-RADS | |||
| 2 | 2 (8%) | 1 | 1 |
| 3 | 3 (12%) | 3 | – |
| 4 | 20 (80%) | 18 | 2 |
Nominal variables are expressed as number and percentage. Scale variables are expressed as median with minimal-maximal values. US, ultrasound; M, mammogram; BI-RADS, Breast Imaging-Reporting and Data System.
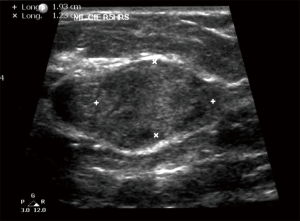
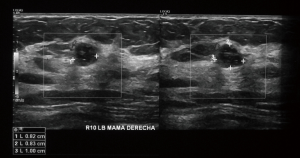
On US study, all asymptomatic cases appeared with a solid nodule. The most frequent US shape of nodules was macrolobular in 19 (76%) (Figure 2), hypoechoic in 16 (64%), and well-circumscribed margins in 18 (72%) cases. Posterior acoustic shadowing was described in 12 (48%), and lateral acoustic shadowing in seven (28%). Only three (12%) cases were register with Doppler vascularity (Figure 3). No large cystic components were observed in these 25 cases. Twenty (80%) of US findings were considered as a score of BI-RADS 4.
Histopathology reports of biopsy and final specimen studies were different between both groups. Diagnoses of fibrocystic breast disease were more frequent in asymptomatic patients (13.6% vs. 1.1%; P=0.001) and diagnoses of phyllodes were fewer (45.5% vs. 63.9%; P=0.001). Diagnosis of fibroadenoma, and not defined fibroepithelial neoplasia were similar. Pseudoangiomatous Stromal Hyperplasia of the breast was reported in six (2.1%) cases among the symptomatic cases. In asymptomatic cases, nine non-palpable PT were treated with local wide-excision guided imaging, four cases with needle-guided excisional biopsy, and five cases, with surgical skin marking.
Discussion
Asymptomatic cases of PT are very rare: at the IEM-FUCAM during a 10-year period, IEM-FUCAM staff diagnosed 346 PT, whose 305 patients were treated (307 tumors), 25 of these were not self-detected. According to the WHO classification (11), the cases included in our study were reported as benign in 72.3%, borderline in 16.3%, and malignant in 11.4%, falling within published ranges for benign (49−74.6%) and borderline (11.2−34.7%) PT, and less frequent than in the series of other authors (9.3−34.7%) (5-7,12,13). In asymptomatic cases, no malignant PT were documented in the present study.
PT usually appear in women with a mean age around 40 years (5,12); the age in our study is within the published range (41.7 years), but asymptomatic cases were older compared with symptomatic ones (47.6±10 vs. 41.2±11.1 years of age, P=0.005). In addition, asymptomatic patients had a higher number of pregnancies (3 vs. 2) and more cases of breastfeeding (80% vs. 61%), these two variables with a statistically significant difference.
The most frequent symptom of PT is a rapid growth nodule identify by the own patient in 60−100% of cases (6,14,15), similar than our findings (91.9%). Small tumors, usually <3 cm are rarely diagnosed and could be detected even smaller in places with breast cancer screening programs, and asymptomatic PT could be as high as 31% (4,10). Park et al. (9) reported a frequency of 25.8% of non-palpable nodules with a mean tumor size of 1.6 cm of the 53 patients with benign PT (data obtained of 6,923 vacuum-assisted breast biopsy). Komenaka et al. (4) reported similar findings; in 2,866 CNB done of US or mammographically detected nodules, they identify 25 PT of the 57 suspicious lumps of this pathology, with an average tumor size of 1.5 cm. Usually asymptomatic cases are reported with a frequency of 2.8–9% (2,8). On other published papers, non-palpable PT has been reported up to 29% (15). In the present study, asymptomatic cases were reported in 25 (8.1%) of the 307 PT treated cases, with a median tumor size of 2.6 cm by US, and 2.1 cm by mammogram. Non-palpable nodules were documented in 3% of all PT, and small non-well identified lumps in 4.9%, very similar to majority of series.
Radiological features of PT are indistinguishable from those of fibroadenomas. Mammographic features are usually characterized by a large, well-circumscribed isodense mass and, on echographic images, PT appear as a smooth, hypoechoic, and solid lobular mass, sometimes with cystic components (1). McCarthy et al. (14) analyzed 54 PTs at their symptomatic breast unit, 50 cases with US lesions and 20 cases with mammographic mass. The US studies identified 86% well defined lesions, 58% lobulated, 58% with pseudocapsule, 46% with heterogeneous internal echogenicity, and 26% with internal cysts. Mammographic studies identified well defined lesion in 60%, obscured margins in 35% and irregular in 5%; visible lobulations in 45%, and the presence of lucent halo in 40%; all these lesions without macro or microcalcification associated. In the present study, in all but one asymptomatic cases, the mammographic images showed a mass without calcifications, and on US studies, all 25 tumors appear as a solid mass, 80% macrolobular, with posterior acoustic shadowing in 48% and hypoechoic or isoechoic US pattern in 88%, without cystic components in these small tumors. Mammography and US cannot be used to differentiate benign from malignant PTs (12). Even there were three cases of Borderline PT, mammographic and US features of the tumor were not different compared to benign ones. Multifocal disease were lower (0.6%) compared to other studies, where were reported as higher than 10% (9). No bilateral disease was reported. Very small tumors could require the use of needle-guided excision for optimal surgical treatment, as occurred in four cases of our series.
In a study of 70 palpable breast lumps suggestive of fibroepithelial tumors, 78.9% of 19 PT, the biopsy were reported has PT, with a Kappa coefficient of 0.81 (16). The concordant rate of diagnosis between CNB and surgical excision in 129 cases with proven PT was 61.2%; the discordance comes from heterogeneous stromal properties of PTs. Diagnostic agreement between CNB and surgical excision had a Kappa value of 0.2196 (3). At the present study, concordant rate of phyllodes diagnosis between CNB and surgical specimen was 45.5% in asymptomatic cases, and 63.9% in symptomatic patients.
In conclusion, asymptomatic cases of PT were documented in 8.1%, and these patients were 6 years older, with more pregnancies, more breastfeeding, with small tumors, compared with symptomatic cases. There is a tendency that asymptomatic cases have more benign PT in a context of postmenopausal patients with higher BMI. Radiological features in asymptomatic cases with PT are indistinguishable from those of fibroadenomas such as well-defined lesions, with macrolobular shape, hypoechoic, and well-circumscribed margins, with low concordant rate between biopsy and definitive histopathological report, so we recommend excisional biopsy in the presence of a low suspicious non-palpable solid nodule even with benign histopathologic report in CNB.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.05.03). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by Institutional Review Board of Instituto de Enfermedades de la Mama and Fundación del Cáncer de Mama (IEM-FUCAM) (No. 16-15) in Mexico City.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Goel NB, Knight TE, Pandey S, et al. Fibrous lesions of the breast: imaging-pathologic correlation. Radiographics 2005;25:1547-59. [Crossref] [PubMed]
- Velázquez-Dohorn M, Gamboa-Domínguez A, Medina-Franco H. Phyllodes tumor of the breast: clinicopathologic analysis of 22 cases. Rev Invest Clin 2013;65:214-20. [PubMed]
- Choi J, Koo JS. Comparative study of histological features between core needle biopsy and surgical excision in phyllodes tumor. Pathol Int 2012;62:120-6. [Crossref] [PubMed]
- Komenaka IK, El-Tamer M, Pile-Spellman E, et al. Core needle biopsy as a diagnostic tool to differentiate phyllodes tumor from fibroadenoma. Arch Surg 2003;138:987-90. [Crossref] [PubMed]
- Wang H, Wang X, Wang CF. Comparison of clinical characteristics between benign borderline and malignant phyllodes tumors of the breast. Asian Pac J Cancer Prev 2014;15:10791-5. [Crossref] [PubMed]
- Ben Hassouna J, Damak T, Gamoudi A, et al. Phyllodes tumors of the breast: a case series of 106 patients. Am J Surg 2006;192:141-7. [Crossref] [PubMed]
- Meneses A, Mohar A, de la Garza-Salazar J, et al. Prognostic factors on 45 cases of phyllodes tumors. J Exp Clin Cancer Res 2000;19:69-73. [PubMed]
- Pérez PJ, Sánchez CG, Bohle OJ, et al. Tumor filodes de la mama. Caracterización clínica e histopatológica de 39 casos. Rev Chil Cir 2007;59:185-90.
- Park HL, Kwon SH, Chang SY, et al. Long-term follow-up result of benign phyllodes tumor of the breast diagnosed and excised by ultrasound-guided vacuum-assisted breast biopsy. J Breast Cancer 2012;15:224-9. [Crossref] [PubMed]
- Pimiento JM, Gadgil PV, Santillan AA, et al. Phyllodes tumors: race-related differences. J Am Coll Surg 2011;213:537-42. [Crossref] [PubMed]
- Lakhani SR, Ellis IO, Schnitt SJ, et al. WHO classification of tumours of the breast. Geneva: International Agency for Research on Cancer, 2012.
- Tan PH. 2005 Galloway Memorial Lecture: Breast phyllodes tumours--morphology and beyond. Ann Acad Med Singapore 2005;34:671-7. [PubMed]
- Reinfuss M, Mituś J, Duda K, et al. The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases. Cancer 1996;77:910-6. [Crossref] [PubMed]
- McCarthy E, Kavanagh J, O'Donoghue Y, et al. Phyllodes tumours of the breast: radiological presentation, management and follow-up. Br J Radiol 2014;87:20140239. [Crossref] [PubMed]
- Youk JH, Kim H, Kim EK, et al. Phyllodes tumor diagnosed after ultrasound-guided vacuum-assisted excision: should it be followed by surgical excision? Ultrasound Med Biol 2015;41:741-7. [Crossref] [PubMed]
- Ricci MD, Amaral PG, Aoki DS, et al. Ultrasound-guided core needle biopsy for the diagnosis of fibroepithelial breast tumors. Rev Bras Ginecol Obstet 2011;33:27-30. [Crossref] [PubMed]
Cite this article as: Ruvalcaba-Limón E, Bautista-Piña V, Villegas-Carlos F, Espejo-Fonseca R, Moguel-Molina N, Tenorio-Torres JA, Rodríguez-Cuevas S. Phyllodes tumor of the breast—not all are self-detected. J Xiangya Med 2017;2:49.