Usage of linear stapler in laparoscopic gastrectomy in gastric cancer patients
In 1994, Kitano et al. first reported the usage of laparoscopic surgery in the treatment of gastric cancer (1). Since then, laparoscopic surgery has been applied in more and more patients and has become an important method of surgery for gastric cancer, especially in East Asia. At first, most of the laparoscopic surgeries for gastric cancer were completed in the way of “laparoscopic-assistant” method, which need a small assistant incision to complete the reconstruction procedures. The advantage of “laparoscopic-assistant” method is that surgeons can perform the reconstruction procedures in the way they are more familiar in open surgery and is easier to master. However, with the development of the laparoscopic techniques, total laparoscopic surgery has become a hot research area (2). For total laparoscopic surgery, reconstruction needs to be performed intracorporeally and this limits the usage of circular stapler which is widely used in open and laparoscopic-assistant surgery. Many techniques have been developed to facilitate the usage of circular stapler in total laparoscopic surgery such as reverse puncture method and trans-oral anvil delivery system (EEATM OrVilTM), but all these techniques are too complicated to be generalized (3). The usage of linear stapler facilitates the development of total laparoscopic surgery. Compared to circular stapler, linear stapler can be inserted into the peritoneal cavity through trocars without assistant incision and the arms of linear stapler can be put into the digestive tract easily which makes it easier to be operated (4). Meanwhile, the procedures with linear stapler have little influence on pneumoperitoneal pressure.
Currently, most of the widely used techniques of total laparoscopic reconstruction methods are completed with linear staplers such as delta anastomosis, esophago-jejunal overlap anastomosis. Since 2013, over 200 cases of reconstructions of gastric cancer surgery were completed with linear staplers in Gastrointestinal Cancer Center of Peking University Cancer Hospital. Here we conclude the usage of linear stapler in reconstruction of gastric cancer surgery and build the basic models of intestinal tract reconstruction method with linear staplers that theoretically exists.
Models of intestinal tract reconstructions with linear staplers
In 1992, Goh et al. first reported total laparoscopic reconstruction of gastro-jejunal anastomosis (5). In 2002, Kanaya et al. first applied total laparoscopic reconstruction techniques in gastric cancer surgery (2). Compared with circular staplers, linear staplers are more suitable for intracorporeal reconstruction. Linear staplers can access the intestinal tract through trocars without assistant incisions and this makes it easier to complete the reconstruction under direct vision of laparoscope. The vision advantage makes sure that the reconstruction is more accurate. The incidence of postoperative intra-abdominal adhesion is low and this facilitates the fast recovery of postoperative bowel function. Besides, most of the circular staplers are with two staple lines while linear staplers are with three staple lines, which is theoretically more accurate and safer.
Although linear staplers can be applied to reconstructions of different anastomosis such as esophago-jejunal, gastro-jejunal, and jejuno-jejunal anastomosis, the basic processes of the procedures are similar. First, a small incision needs to be made at the antimesenteric border of each of the two intestinal tracts. Then the two arms of the linear stapler are inserted into the two intestinal tracts separately. Finally, the linear stapler is fired and the conjunct incision is closed. The basic procedures of different anastomosis are similar but the details vary. Here we concluded the basic forms of the procedure and modelled it. Theoretically, we introduced all the forms procedures that might exist and analyzed them together with clinical practice.
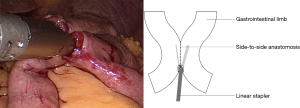
- Basic form (Figure 1): the nature of reconstructions with linear stapler is the side-to side anastomosis. Two arms of the stapler are inserted into two different intestinal tracts like showing in Figure 1. Both intestinal tracts are not transected and there are four limbs and no cutting lines around the anastomoses. In clinical practice, jejuno-jejunal anastomosis (Braun anastomosis) and gastro-jejunal bypass anastomosis are of this specific form (6).
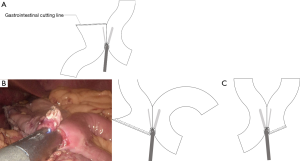
- One limb transected (Figure 2): one lime around the anastomoses is transected and thus there are three limbs and one cutting line around the anastomoses. According to the directions of linear stapler inserted into the intestinal tract, there are two subtypes of this form.
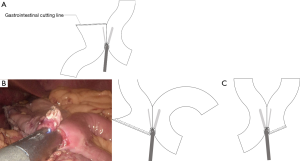 Figure 2 One limb transected. (A) Inserting the stapler arms away from the cutting line (gastro-jejunal anastomosis); (B) inserting the stapler arms on the cutting line (gastro-jejunal anastomosis); (C) inserting the stapler arms on the cutting line (jejuno-jejunal anastomosis).
Figure 2 One limb transected. (A) Inserting the stapler arms away from the cutting line (gastro-jejunal anastomosis); (B) inserting the stapler arms on the cutting line (gastro-jejunal anastomosis); (C) inserting the stapler arms on the cutting line (jejuno-jejunal anastomosis).- In the first subtype, the small incisions are made away from the cutting line and the linear stapler is inserted towards the line, like showing in Figure 2A. In clinical practice, the remnant gastro-jejunal anastomosis in double-tract reconstruction of proximal gastrectomy is of this specific subtype.
- In the second subtype, the small incisions are made on the cutting line, like showing in Figure 2B,C. In clinical practice, the gastro-jejunal anastomosis in Billroth II reconstruction of distal gastrectomy (Figure 2B), the jejuno-jejunal anastomosis in Roux-en-Y reconstruction of distal or total gastrectomy and in double-tract reconstruction of proximal gastrectomy (Figure 2C) are of this specific subtype.
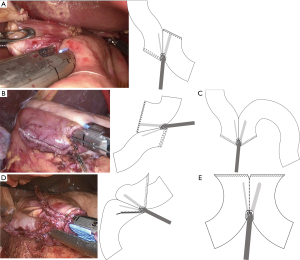
- Two limbs transected (Figure 3): two limbs around the anastomosis are transected, and there are two limbs and two cutting lines left around the anastomoses. According to the distribution of the left limbs, there are two subtypes of this form.
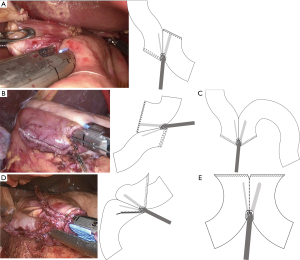 Figure 3 Two limbs transected. (A) Two limbs left at different side of the anastomosis (esophago-jejunal overlap anastomosis); (B) two limbs left at different side of the anastomosis (gastro-duodenal overlap anastomosis); (C) two limbs at the same side of the anastomosis and the stapler arms inserted on the cutting line (esophago-jejunal FETE anastomosis); (D) two limbs at the same side of the anastomosis and the stapler arms inserted on the cutting line (gastro-duodenal delta anastomosis); (E) two limbs at the same side of the anastomosis and the stapler arms inserted away from the cutting line. FETE, functional end-to-end.
Figure 3 Two limbs transected. (A) Two limbs left at different side of the anastomosis (esophago-jejunal overlap anastomosis); (B) two limbs left at different side of the anastomosis (gastro-duodenal overlap anastomosis); (C) two limbs at the same side of the anastomosis and the stapler arms inserted on the cutting line (esophago-jejunal FETE anastomosis); (D) two limbs at the same side of the anastomosis and the stapler arms inserted on the cutting line (gastro-duodenal delta anastomosis); (E) two limbs at the same side of the anastomosis and the stapler arms inserted away from the cutting line. FETE, functional end-to-end.- In the first subtype, the two limbs left are at the different side of the anastomoses (Figure 3A,B). In this subtype, the small incision is made on one of the cutting line and then the linear stapler is inserted. As this subtype of anastomoses is central symmetrical, the direction of linear stapler inserted does not change the formation of the anastomoses. In clinical practice, this subtype is usually called “overlap” anastomoses and is generally used in esophago-jejunal anastomosis of total gastrectomy (Figure 3A) and gastro-duodenal anastomosis of distal gastrectomy (Figure 3B) (7).
- In the second subtype, the two limbs left are at the same side of the anastomoses (Figure 3C-E). In this subtype, linear stapler can be inserted in two different directions. In the first one, the small incision is made on the cutting line and the linear stapler is inserted towards the direction of the left limbs, like showing in Figure 3C,D. In clinical practice, functional end-to-end esophago-jejunal anastomosis (FETE) of total gastrectomy (Figure 3C) and gastro-duodenal delta anastomosis of distal gastrectomy are of this specific form (8). In the second one, the small incisions are made away from the cutting line and the linear stapler is inserted towards the cutting line, like showing in Figure 3E. However, this method exists theoretically and currently is not applied in clinical practice.
Above are all the theoretically existing forms of anastomosis by linear stapler. In clinical practice, the specific anastomoses are modified on the basis of these forms. The modified factors include the direction of stapler inserted, symmetry variation, selection of intestinal tract wall for side-to-side anastomoses, direction of intestinal tract transection, methods of conjunct incision closure, and selection of stapler size. For example, in delta anastomoses reported by Kanaya (Figure 3D), the details modified on the basis of theoretical form are as follows: the direction of duodenum transection is from back wall to front wall; the intestinal walls selected for side-to-side anastomoses are back wall of gastric wall and upper wall of duodenum; the conjunct incision is closed with another linear stapler and the closure line forms the anastomoses a delta shape (2). Huang et al. modified the traditional delta anastomosis by moving away the duodenal stump cutting line while closing the conjunct incision (9).
The modification of details of anastomosis will bring different effect. For example, the direction of linear stapler inserted into the intestinal tract is modified according to the position of the surgeon and the relative location and direction of the intestinal tract. The intestinal tract wall for anastomosis is selected according to the blood supply, mobilization, and adjacent organs of the intestinal tract wall. The closure of the conjunct incision can be performed with linear stapler or hand-sewing according to the mobilization of the tract. Laparoscopic hand-sewing technique is more complicated and requires more experience while the application of barbed sutures facilitates the procedure a lot. The closure of conjunct incision with linear staplers is easier but requires more space and thus need the tract to be more mobilized. It is usually applied in gastro-jejunal, jejuno-jejunal anastomosis but not in esophago-jejunal anastomosis. The direction to close the conjunct incision will influence the diameter of the anastomosis. If the closure line forms the delta shape with the anastomosis lines, the anastomosis are with lower possibility of stricture. Meanwhile, the size of linear stapler selected will also influence the diameter of the tract.
In summary, the usage of linear staplers in reconstruction is acceptable from the aspects of operation time, bowel function recovery, and postoperative morbidity. Due to the simpler process of the procedure and the basic procedures are similar in different anastomosis, the learning curve of the procedure is shorter and resulted in better operation safety. It is worthy to generalize the usage of it. With all these advantages, our center has begun to apply linear stapler in reconstruction in open surgery. The models we introduced here can provide experiences for clinical practice of linear stapler in reconstruction of gastrectomy.
Acknowledgments
Funding: None.
Footnote
Provenance and Peer Review: This article was a standard submission to the journal. The article did not undergo external peer review.
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.04.02). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kitano S, Iso Y, Moriyama M, et al. Laparoscopy-assisted Billroth I gastrectomy. Surg Laparosc Endosc 1994;4:146-8. [PubMed]
- Kanaya S, Gomi T, Momoi H, et al. Delta-shaped anastomosis in totally laparoscopic Billroth I gastrectomy: new technique of intraabdominal gastroduodenostomy. J Am Coll Surg 2002;195:284-7. [Crossref] [PubMed]
- Jeong O, Park YK. Intracorporeal circular stapling esophagojejunostomy using the transorally inserted anvil (OrVil) after laparoscopic total gastrectomy. Surg Endosc 2009;23:2624-30. [Crossref] [PubMed]
- Okabe H, Obama K, Tsunoda S, et al. Advantage of completely laparoscopic gastrectomy with linear stapled reconstruction: a long-term follow-up study. Ann Surg 2014;259:109-16. [Crossref] [PubMed]
- Goh P, Tekant Y, Kum CK, et al. Totally intra-abdominal laparoscopic Billroth II gastrectomy. Surg Endosc 1992;6:160. [Crossref] [PubMed]
- Uyama I, Sakurai Y, Komori Y, et al. Laparoscopy-assisted uncut Roux-en-Y operation after distal gastrectomy for gastric cancer. Gastric Cancer 2005;8:253-7. [Crossref] [PubMed]
- Byun C, Cui LH, Son SY, et al. Linear-shaped gastroduodenostomy (LSGD): safe and feasible technique of intracorporeal Billroth I anastomosis. Surg Endosc 2016;30:4505-14. [Crossref] [PubMed]
- Okabe H, Obama K, Tanaka E, et al. Intracorporeal esophagojejunal anastomosis after laparoscopic total gastrectomy for patients with gastric cancer. Surg Endosc 2009;23:2167-71. [Crossref] [PubMed]
- Huang CM, Lin M, Lin JX, et al. Comparision of modified and conventional delta-shaped gastroduodenostomy in totally laparoscopic surgery. World J Gastroenterol 2014;20:10478-85. [Crossref] [PubMed]
Cite this article as: Li Z, Miao R. Usage of linear stapler in laparoscopic gastrectomy in gastric cancer patients. J Xiangya Med 2017;2:36.