Clinical research of totally laparoscopic modified Roux-en-Y reconstruction
Introduction
For more than 20 years, laparoscopic gastric cancer surgery progressed worldwide (1,2), which totally laparoscopic gastric surgery and gastrointestinal tract reconstruction is one of the most complex procedure. The operation team with a higher level of minimally invasive techniques should be needed. Types of laparoscopic gastrointestinal tract reconstruction after total gastrectomy are various, mainly includes the application of the circular anastomosis and the linear anastomosis (3). The most common used for laparoscopic digestive tract reconstruction after total gastrectomy is Roux-en-Y anastomosis, which is nearly the same procedure as the open surgery to dissect a loop of intestine with blood arch. It’s important to simplify this procedure because the small intestine mesentery dissected totally laparoscopically is inconvenient. Based on the traditional Roux-en-Y anastomosis modified, without small intestinal mesentery dissection, the Roux-en-Y anastomosis can be completely performed. Comparing the classic and modified Roux-en-Y anastomosis, a simple technique should be valued for the totally laparoscopic gastrointestinal tract reconstruction after total gastrectomy.
Methods
Patients
We retrospectively reviewed the medical records of 36 patients who underwent totally laparoscopic total gastrectomy (TLTG) with Roux-en-Y reconstruction in the second hospital of Jilin University between January 2014 and December 2014. There were 21 males and 15 females. The indication of TLTG included the patients with gastric adenocarcinoma located on the upper, upper to middle, or entire stomach, who were tested by endoscopy and abdominal CT scan. All operations were performed by one team of surgeon. All of the patients provided written informed consent to participate in the study. This study is also approved by the Ethics Committee of the Second Hospital of Jilin University.
Surgical technique
Under general anesthesia, the patient was placed in the supine position split with legs and the camera operator standing between. The chief surgeon was positioned on the left side of the patient and the first assistant on the right side of the patient during stomach mobilization and lymph nodes dissection. Five trocars were inserted as showed in Figure 1. After stomach mobilization and lymph nodes dissection, the esophagus and duodenal should be transected with an endoscopic linear. The resected specimen were placed in a plastic specimen bag and retrieved through the umbilical trocar extended incision (Figure 1). Then the pneumoperitoneum was re-established by suturing the umbilical incision to the size of the trocar, the surgeon and the first assistant switched their positions for the later gastrointestinal tract reconstruction as needed.

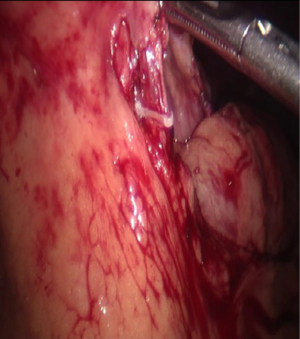
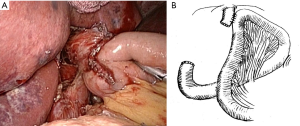
Laparoscopic classic Roux-en-Y reconstruction (CRY): 16 cases
First, the dissection of the mesentery was created (Figure 2), then the jejunum was transected 15–20 cm distal to the Treitz’s ligament by using an endoscopic linear. The distal side of the jejunum (approximately 3–5 cm long) was usually removed avoiding excessive tension and lack of mesenteric blood supply. The side to side esophagojejunostomy was performed at the left side of esophagus by endoscopic linear in an ante-colic fashion (Figure 2). In case of false anastomosis, the fork of the linear stapler inserted into the hole of the esophagus was always guided by a nasogastric tube. The entry hole was created after a side-to-side esophagojejunostomy and closed by a continuous hand-sewn technique. At the lumen 40–50 cm distal from the esophagojejunostomy, a side-to-side jejuno-jejunostomy was performed intracorporeally, and the entry hole was also closed by using a continuous hand-sewn technique.
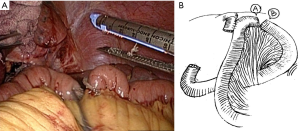
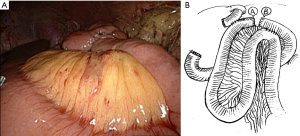
Laparoscopic modified Roux-en-Y reconstruction (MRY): 20 cases
The side-to-side esophagojejunostomy was performed directly by one fork of the endoscopic stapler inserted into the jejunum 15–20 cm distal to the Treitz’s ligament, another fork inserted carefully into the hole of the esophagus guided by nasogastric tube (Figure 3). After firing of the stapler converted the two openings into a single entry hole. The entry hole was closed by a continuous hand-sewn technique. The jejunum distal to the esophagojejunostomy 2–3 cm was intracorporeally transected and the mesenteric dissection was not needed (Figure 4). A side to side jejuno-jejunostomy was performed as described above (Figure 5).
Clinicopathological findings
All the patients information, including gender, age, body mass index (BMI), operative duration, blood loss, number of lymph nodes dissection, pathological findings, and perioperative complications was collected. All values are expressed as means ± standard deviation.
Results
All 36 patients were successfully completed totally laparoscopically, there was no conversion from laparoscopic surgery to open surgery. Table 1 shows the clinicopathologic characteristics of the study groups. The age, sex ratio, BMI, history of abdominal surgery, tumor diameter and TNM staging did not differ between the CRY group (20 cases) and MRY group (16 cases).
Table 1
| Characteristic | MRY (n=20) | CRY (n=16) | P value |
|---|---|---|---|
| Age (years) | 57.4±10.3 | 56.7±11.9 | 0.851 |
| Male/female | 10/10 | 10/6 | 0.517 |
| BMI (kg/m2) | 22.2±2.3 | 21.9±4.5 | 0.797 |
| History of abdominal surgery (n) | 5 (25.0%) | 3 (18.8%) | 0.654 |
| Tumor size (cm) | 5.2±1.3 | 4.9±0.7 | 0.413 |
| TNM stage (n) | 0.189 | ||
| I | 2 (10.0%) | 1 (6.2%) | |
| II | 6 (30.0%) | 4 (25.0%) | |
| III | 12 (60.0%) | 11 (68.8%) |
MRY, modified Roux-en-Y reconstruction; CRY, classic Roux-en-Y reconstruction.
The perioperative data were summarized in Table 2. The operative time was 260.9±21.2 mins in the MRY group and 287.9±19.0 min in the CRY group, and the blood loss was less than the CRY group (50.9±23.5 vs. 67.0±20.5 mL; P=0.01). The number of dissected lymph nodes did not differ between the study groups. The Roux-en-Y reconstruction time was 32.4±9.2 min in the MRY group and 45.4±13.2 min in the CRY group. The length of the mesenteric dissection and the removed intestine were 11.6±4.5 and 3.6±2.3 cm in the CRY group. The time to flatus, postoperative hospitalization and the complications did not differ between the study groups.
Table 2
| Characteristic | MRY (n=20) | CRY (n=20) | P value |
|---|---|---|---|
| Operative time (min) | 260.9±21.2 | 287.9±19.0 | 0.000 |
| Blood loss (mL) | 50.9±23.5 | 67.0±20.5 | 0.000 |
| Reconstruction time (min) | 32.4±9.2 | 45.4±13.2 | 0.001 |
| No. of dissected lymph nodes | 33.4±6.5 | 34.3±8.2 | 0.715 |
| Length of mesentery dissection (cm) | 0 | 11.6±4.5 | 0.000 |
| Length of removed intestine (cm) | 0 | 3.6±2.3 | 0.000 |
| Flatus time (days) | 2.8±1.5 | 3.0±0.9 | 0.642 |
| Postoperative hospital stay (days) | 7.3±4.5 | 8.1±6.5 | 0.666 |
| Postoperative complications (n) | 3 (15.0) | 4 (28.6) | 0.783 |
| Ileus | 1 | 1 | |
| Anastomotic leakage | 0 | 1 | |
| Gastrointestinal bleeding | 1 | 1 | |
| Duodenal fistula | 0 | 0 | |
| Incision infection | 0 | 1 | |
| Alkaline reflux gastritis | 1 | 0 |
MRY, modified Roux-en-Y reconstruction; CRY, classic Roux-en-Y reconstruction
Discussion
Laparoscopic surgery is widely used for gastric cancer due to its minimal invasiveness. The related technique is always mastered by the experienced surgeons. Totally laparoscopic gastrectomy (TLG), however, is not widely accepted because of its technical difficulty in comparison with laparoscopic assisted gastrectomy (LAG). In particular, the intracorporeal gastrointestinal tract reconstruction after total gastrectomy for gastric cancer is thought to be particularly difficult (4,5). Currently, various methods of intracorporeal gastrointestinal tract reconstruction are normally used and the Roux-en-Y reconstruction accepted widely, which is a method of side-to-side EJ (esophagojejunal) anastomosis using a linear stapler. To overcome the difficulties of intracorporeal esophagojejunostomy and simplify the process, we tried to develop a novel method described here. In this study, the short-time effect did not differ between the MRY group and CRT group.
In 1999, Uyama et al. (6) first reported laparoscopic side-to-side anastomosis by the endo linear cutters. As most surgeon preformed, however, the jejunum and the esophagus were transected, the mesentery was dissected before the esophagojejunal anastomosis. In recent years, with the development of the laparoscopic instruments and skills, various of the gastrointestinal tract reconstruction after laparoscopic total gastrectomy performed by the experienced surgeons. Noh et al. (7) reported a laparoscopic purse-string suture in the distal esophagus and inserting an anvil, but laparoscopic endo linear anastomosis accepted more widely, such as Billoth I delta anastomosis and Roux-en-Y uncut anastomosis (3,8,9). Roux-en-Y anastomosis is usually used after total gastrectomy, various of modified Roux-en-Y anastomosis appeared in the recent year. At the beginning, the mini-incision was prepared by the surgeon for the reconstruction, but it was complicated as the larger incision, blur surgical vision and more blood for the fat patients, so the recent studies suggested that intracorporeal anastomosis is more benefit than extracorporeal anastomosis. In 2009, Okabe et al. (10) reported a new technique to fulfill the intracorporeal linear-stapled esophagojejunal anastomosis, which can be performed safely and easily. The entire procedure was performed totally under laparoscopy, the method could be applied easily to obese patients. They also made some improvement: linear stapled esophagojejunostomy in the left side cause of sufficient free work space, insertion of an endoscopic linear fork into the true lumen of the esophagus guided by nasogastric tube. Inaba et al. (11) also previously reported the intracorporeal esophagojejunostomy by functional end-to-end anastomosis using an endoscopic linear stapler. In 2013, Shim and his teammates (12) summarized various types of anastomosis after LTG and evaluated the postoperative surgical outcomes according to their four types of anastomosis. Each study described the mesentery should be dissected and the jejunum should be transected for the Roux-en Y anastomosis (13). As far as we know, this is the first report that mesenteric does not need to be dissected for the Roux-en Y anastomosis after LTG.
At the beginning of the study, we performed this modified Roux-en Y anastomosis for the open surgery after the total gastrectomy. We started to perform the intracorporeal anastomosis after the learning curve completed and the laparoscopic techniques developed. This modified Roux-en Y anastomosis has several advantages: (I) shorten the reconstruction time to shorten the operation time; (II) the dissection of the mesentery of the jejunum and the jejunum resection were not needed; (III) no stitches were made to close the dissected mesentery. As compared with the classic Rou-en-Y anastomosis, the modified group is associated with the same short-term clinical outcomes. With all these modifications, our new procedure could become one of the simple, economic, feasible and safe procedures for intracorporeal gastrointestinal tract reconstruction after LTG.
However, further clinical and randomized controlled trials are needed to evaluate its long-term effects. This study was limited by its small patient population. To launch this new method, an experienced laparoscopic work team should be necessary.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2017.04.06). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). All of the patients provided written informed consent to participate in the study. This study is also approved by the Ethics Committee of the Second Hospital of Jilin University.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Kitano S, Shiraishi N, Uyama I, et al. A multicenter study on oncologic outcome of laparoscopic gastrectomy for early cancer in Japan. Ann Surg 2007;245:68-72. [Crossref] [PubMed]
- Mochiki E, Kamiyama Y, Aihara R, et al. Laparoscopic assisted distal gastrectomy for early gastric cancer: Five years' experience. Surgery 2005;137:317-22. [Crossref] [PubMed]
- Kim JJ, Song KY, Chin HM, et al. Totally laparoscopic gastrectomy with various types of intracorporeal anastomosis using laparoscopic linear staplers: preliminary experience. Surg Endosc 2008;22:436-42. [Crossref] [PubMed]
- Bracale U, Marzano E, Nastro P, et al. Side-to-side esophagojejunostomy during totally laparoscopic total gastrectomy for malignant disease: a multicenter study. Surg Endosc 2010;24:2475-9. [Crossref] [PubMed]
- Ebihara Y, Okushiba S, Kawarada Y, et al. Outcome of functional end-to-end esophagojejunostomy in totally laparoscopic total gastrectomy. Langenbecks Arch Surg 2013;398:475-9. [Crossref] [PubMed]
- Uyama I, Sugioka A, Fujita J, et al. Laparoscopic total gastrectomy with distal pancreatosplenectomy and D2 lymphadenectomy for advanced gastric cancer. Gastric Cancer 1999;2:230-4. [Crossref] [PubMed]
- Noh SY, Lee JH, Ahn SH, et al. Intracorporeal End-to-Side Esophagojejunostomy Using a Laparoscopic Purse-String Clamp during Laparoscopic Total Gastrectomy. J Minim Invasive Surg 2012;15:32-7. [Crossref]
- Man-I M, Suda K, Kikuchi K, et al. Totally intracorporeal delta-shaped B-I anastomosis following laparoscopic distal gastrectomy using the Tri-Staple™ reloads on the manual Ultra handle: a prospective cohort study with historical controls. Surg Endosc 2015;29:3304-12. [Crossref] [PubMed]
- Yun SC, Choi HJ, Park JY, et al. Total laparoscopic uncut Roux-en-Y gastrojejunostomy after distal gastrectomy. Am Surg 2014;80:E51-3. [PubMed]
- Okabe H, Obama K, Tanaka E, et al. Intracorporeal esophagojejunal anastomosis after laparoscopic total gastrectomy for patients with gastric cancer. Surg Endosc 2009;23:2167-71. [Crossref] [PubMed]
- Inaba K, Satoh S, Ishida Y, et al. Overlap method: novel intracorporeal esophagojejunostomy after laparoscopic total gastrectomy. J Am Coll Surg 2010;211:e25-9. [Crossref] [PubMed]
- Shim JH, Yoo HM, Oh SI, et al. Various types of intracorporeal esophagojejunostomy after laparoscopic total gastrectomy for gastric cancer. Gastric Cancer 2013;16:420-7. [Crossref] [PubMed]
- Ziqiang W. A modified method of laparoscopic side-to-side esophagojejunal anastomosis: report of 14 cases. Surg Endosc 2008;22:2091-4. [Crossref] [PubMed]
Cite this article as: Liu T, Ma Z, Fang X, Zhu J. Clinical research of totally laparoscopic modified Roux-en-Y reconstruction. J Xiangya Med 2017;2:8.