Computed tomography, electronic health record, and private medical cloud—impact of information technology on clinical decision making
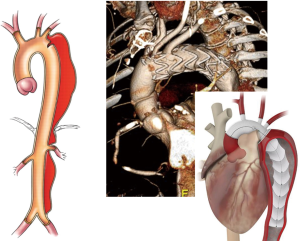
The introduction of computed tomography (CT) to medical imaging in the 1970’s has had significant impact on clinical decision making across specialties in medicine and surgery (1). CT has replaced other imaging modalities e.g., in the assessment of acute aortic dissection and pulmonary embolism. Importantly, because of its 3-dimensional data structure, it is superior for planning of minimally invasive surgical and endovascular procedures (2). In fact, CT has been an integral part of the development of endovascular stent treatment of aortic disease and novel transcatheter procedures for valvular and structural heart disease (3,4).
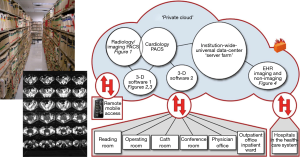
CT imaging is based on complex digital data acquisition and analysis, which became possible by advances in computer sciences. These advances in digital data storage and analysis have changed communication and data sharing in medicine. Over the last few decades the traditional paper medical record and printed X-ray films have been replaced by electronic medical records (EMR) and digital image review on computer workstations, respectively (5,6) (Figure 1). This has had significant impact on clinical decision making, exemplified by the management of acute aortic syndromes (AAS) and transcatheter aortic valve replacement (TAVR). In the case of AAS, immediate availability across a healthcare system supports rapid communication within a group of specialists supports emergent management. In the case of TAVR sharing of images across sub-specialties supports planning of the elective procedure.
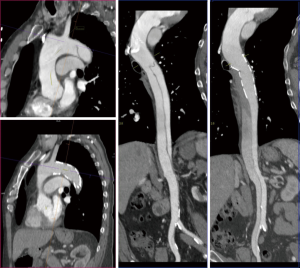
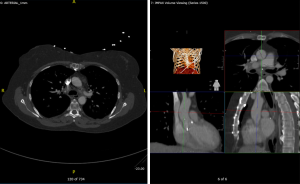
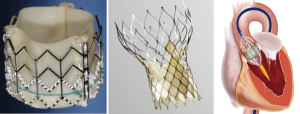
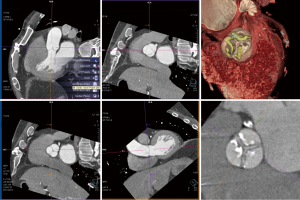
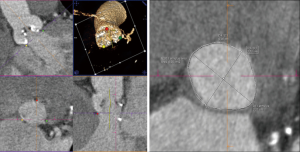
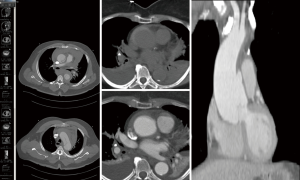
Severe aortic stenosis is common in elderly patient and the only definitive treatment is aortic valve replacement (7). Less invasive TAVR has developed into a viable alternative to conventional open heart surgery for patient with high surgical risk (8,9) (Figure 2). More recent results demonstrate its clinical value in intermediate risk populations (10). Because of the lack of direct, intra-operative visualization of the valve and annulus, pre-procedural imaging including CT imaging is fundamental for indication and procedural planning (Figure 3). Specifically the reconstruction and analysis of the aortic annulus and evaluation of access vessels is a critical (Figure 4) (11,12). Data collected during history taking, physical examination and from laboratory and imaging studies are combined in the EMR and shared between multiple specialists in clinical and interventional cardiology, radiology, anesthesiology, surgery, nursing, etc. Availability at different times and multiple locations during pre-procedural evaluation, and peri- and post-procedural management is necessary (Figure 5).

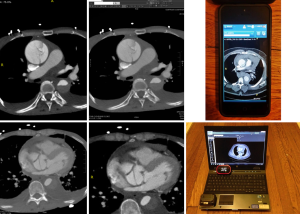
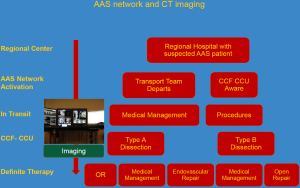
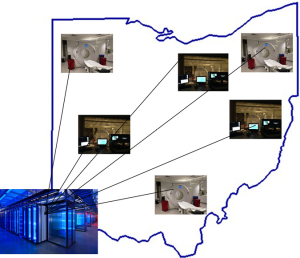
AAS/dissections are medical/surgical emergencies, associated with significant mortality. Early diagnosis and treatment is critical (13,14) (Figures 6,7,8). Early CT imaging, which is typically performed at the point of initial contact in the emergency department is critical for definitive diagnosis. After initial diagnosis, patients are often immediately transferred to a tertiary center for definitive management (15,16). Emergent imaging and sharing of the imaging data is critical in the time period between initial presentation and definitive management (Figure 9). A shared ‘private medical cloud’ maintained from a central server farm/data center is an attractive solution (Figure 10).
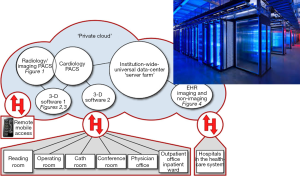
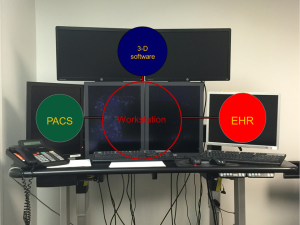
The architecture of such IT networks includes scanners spread across a larger geographical region, which feed data into a shared picture archiving and communication system (PACS) as part of the medical cloud (Figure 11). This makes the images available from the central archive from workstations across the entire health care system. Access is possible with a high end workstation e.g., located in a reading room, which provides access to basic PACS review but also dedicated 3-D reconstruction with one or more software (Figure 12). On the other hand review of images is also possible via basic EMR workstations anywhere within the health-care system by any user with access privileges (Figure 13). Access is also possible from mobile devices (Figure 14) creating a mobile network of specialists (Figure 15) (17).
If such data networks are combined with ‘smart workstations’ and machine learning, they can provide decision support (18-20).
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: Both authors have completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/jxym.2016.12.14). PS serves as the Editor-in-Chief of Journal of Xiangya Medicine. HL has no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Hounsfield GN. Computerized transverse axial scanning (tomography). 1. Description of system. Br J Radiol 1973;46:1016-22. [Crossref] [PubMed]
- Schoenhagen P, Numburi U, Halliburton SS, et al. Three-dimensional imaging in the context of minimally invasive and transcatheter cardiovascular interventions using multi-detector computed tomography: from pre-operative planning to intra-operative guidance. Eur Heart J 2010;31:2727-40. [Crossref] [PubMed]
- Kitagawa A, Greenberg RK, Eagleton MJ, et al. Fenestrated and branched endovascular aortic repair for chronic type B aortic dissection with thoracoabdominal aneurysms. J Vasc Surg 2013;58:625-34. [Crossref] [PubMed]
- Schoenhagen P, Hausleiter J, Achenbach S, et al. Computed tomography in the evaluation for transcatheter aortic valve implantation (TAVI). Cardiovasc Diagn Ther 2011;1:44-56. [PubMed]
- Hughes J. NSW public hospitals accessing digital radiology images. Cardiovasc Diagn Ther 2012;2:E14-5. [PubMed]
- Schoenhagen P, Falkner J, Piraino D. Transcatheter aortic valve repair, imaging, and electronic imaging health record. Curr Cardiol Rep 2013;15:319. [Crossref] [PubMed]
- Nkomo VT, Gardin JM, Skelton TN, et al. Burden of valvular heart diseases: a population-based study. Lancet 2006;368:1005-11. [Crossref] [PubMed]
- Kapadia SR, Leon MB, Makkar RR, et al. 5-year outcomes of transcatheter aortic valve replacement compared with standard treatment for patients with inoperable aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet 2015;385:2485-91. [Crossref] [PubMed]
- Mack MJ, Leon MB, Smith CR, et al. 5-year outcomes of transcatheter aortic valve replacement or surgical aortic valve replacement for high surgical risk patient with aortic stenosis (PARTNER 1): a randomised controlled trial. Lancet. 2015;385:2477-84. [Crossref] [PubMed]
- Arora S, Misenheimer JA, Jones W, et al. Transcatheter versus surgical aortic valve replacement in intermediate risk patients: a meta-analysis. Cardiovasc Diagn Ther 2016;6:241-9. [Crossref] [PubMed]
- Achenbach S, Delgado V, Hausleiter J, et al. SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr 2012;6:366-80. [Crossref] [PubMed]
- Lou J, Obuchowski NA, Krishnaswamy A, et al. Manual, semiautomated, and fully automated measurement of the aortic annulus for planning of transcatheter aortic valve replacement (TAVR/TAVI): analysis of interchangeability. J Cardiovasc Comput Tomogr 2015;9:42-9. [Crossref] [PubMed]
- Braverman AC. Aortic dissection: prompt diagnosis and emergency treatment are critical. Cleve Clin J Med 2011;78:685-96. [Crossref] [PubMed]
- Svensson LG, Labib SB, Eisenhauer AC, et al. Intimal tear without hematoma: an important variant of aortic dissection that can elude current imaging techniques. Circulation 1999;99:1331-6. [Crossref] [PubMed]
- Aggarwal B, Raymond CE, Randhawa MS, et al. Transfer metrics in patients with suspected acute aortic syndrome. Circ Cardiovasc Qual Outcomes 2014;7:780-2. [Crossref] [PubMed]
- Raymond CE, Aggarwal B, Schoenhagen P, et al. Prevalence and factors associated with false positive suspicion of acute aortic syndrome: experience in a patient population transferred to a specialized aortic treatment center. Cardiovasc Diagn Ther 2013;3:196-204. [PubMed]
- Schoenhagen P, Zimmermann M, Falkner J. Advanced 3-D analysis, client-server systems, and cloud computing-Integration of cardiovascular imaging data into clinical workflows of transcatheter aortic valve replacement. Cardiovasc Diagn Ther 2013;3:80-92. [PubMed]
- Matar R, Renapurkar R, Obuchowski N, et al. Utility of hand-held devices in diagnosis and triage of cardiovascular emergencies. Observations during implementation of a PACS-based system in an acute aortic syndrome (AAS) network. J Cardiovasc Comput Tomogr 2015;9:524-33. [Crossref] [PubMed]
- Schoenhagen P, Roselli EE, Harris CM, et al. Online network of subspecialty aortic disease experts: Impact of "cloud" technology on management of acute aortic emergencies. J Thorac Cardiovasc Surg 2016;152:39-42. [Crossref] [PubMed]
- Schoenhagen P, Mehta N. Big data, smart computer systems, and doctor-patient relationship. Eur Heart J 2016; [Epub ahead of print]. [Crossref] [PubMed]
Cite this article as: Schoenhagen P, Liu H. Computed tomography, electronic health record, and private medical cloud—impact of information technology on clinical decision making. J Xiangya Med 2016;1:14.